 HealthLawBlog will be on vacation for the next two weeks.
HealthLawBlog will be on vacation for the next two weeks. With random exceptions, don't expect anything new here before August 10th.
Stay cool. Be happy.
Health care law (including regulatory and compliance issues, public health law, medical ethics, and life sciences), with digressions into constitutional law, statutory interpretation, poetry, and other things that matter
 Today's CDC Public Health Law Newsletter has a link to a Chicago Tribune article that explores the ethics of triage and its applicability vel non to the NOLA cases previously discussed (here, here, and here):
Today's CDC Public Health Law Newsletter has a link to a Chicago Tribune article that explores the ethics of triage and its applicability vel non to the NOLA cases previously discussed (here, here, and here):“Disaster plan: Time to think unthinkable?”
Chicago Tribune (07/19/06) Ronald Kotulak
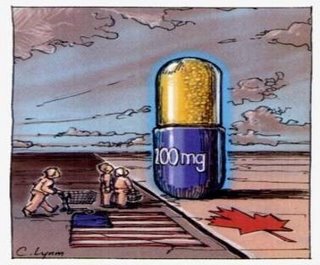
Last week, two nurses and a doctor were arrested in New Orleans on charges that they gave lethal doses of drugs to four hospital patients in the aftermath of Hurricane Katrina. The second-degree murder charges have led ethicists to begin debating what actions taken by medical personnel are permissible in similar situations, such as catastrophic weather events, deployments of weapons of mass destruction, or even widespread influenza epidemics. In such situations, medical care might be limited. “What do you do if you had no way to treat people and they were ill and there was no power and the ventilation had gone down and the machines that had kept them alive were failing? That is an astonishingly important ethical problem, given the realities we face with disaster planning,” said Laurie Zoloth, director of the Center for Bioethics, Science and Society at the Northwestern University Feinberg School of Medicine. Zoloth compared such scenarios to doctors triaging wounded soldiers on the battlefield. Dr. Mark Siegler of the University of Chicago’s MacLain Center for Medical Ethics said there is sometimes a fine line between giving a patient morphine for pain and a dose high enough to cause death. But Dr. Joshua Hauser, a palliative care expert, said doctors have specific guidelines to follow to avoid a morphine-related death. “There’s significant consensus in the medical community that giving a dose of morphine with the intent of ending someone’s life is unacceptable,” he said.
 As previously noted, the Senate has passed a bill that would impose criminal penalties on anyone who helps a minor travel across state lines from a state that has a parental-notification or -consent law in order to obtain an abortion in a state that has no such restrictions. As the map on my post illustrates, 6 states have no restrictions on minors: Washington, Oregon, Vermont, New York, Massachusetts, and Hawai'i. The House previously passed a similar bill [H.R.748; roll call #144], and news reports today say the president has said he will sign a bill if the two houses of Congress can agree on language in conference [NY Times].
As previously noted, the Senate has passed a bill that would impose criminal penalties on anyone who helps a minor travel across state lines from a state that has a parental-notification or -consent law in order to obtain an abortion in a state that has no such restrictions. As the map on my post illustrates, 6 states have no restrictions on minors: Washington, Oregon, Vermont, New York, Massachusetts, and Hawai'i. The House previously passed a similar bill [H.R.748; roll call #144], and news reports today say the president has said he will sign a bill if the two houses of Congress can agree on language in conference [NY Times]. The Washington Post has the story. The Senate has passed a a bill (S.403) "to prohibit taking minors across State lines in circumvention of laws requiring the involvement of parents in abortion decisions [preamble]," thus (according to The Post) handing a long-sought victory to the Bush administration and abortion opponents":
The Washington Post has the story. The Senate has passed a a bill (S.403) "to prohibit taking minors across State lines in circumvention of laws requiring the involvement of parents in abortion decisions [preamble]," thus (according to The Post) handing a long-sought victory to the Bush administration and abortion opponents":The Senate bill is here and the roll-call vote is here.The bill would help about three dozen states enforce laws that require minors to notify or obtain the consent of their parents before having an abortion. It would bar people -- including clergy members and grandparents -- from helping a girl cross state lines to avoid parental-involvement laws. Violations could result in a year in prison.
Most states have passed such laws, but courts
have invalidated at least nine of them, advocacy groups say. . . . The Senate voted 65 to 34 to approve the bill, which is similar to one the House has approved before, including last year.
 Starchild Abraham Cherrix has Hodgkin's disease, and when the disease returned after his initial round of chemo, he refused a second round, opting instead for "a sugar-free, organic diet and take herbal supplements under the supervision of a clinic in Mexico" [Washington Post]:
Starchild Abraham Cherrix has Hodgkin's disease, and when the disease returned after his initial round of chemo, he refused a second round, opting instead for "a sugar-free, organic diet and take herbal supplements under the supervision of a clinic in Mexico" [Washington Post]:A social worker asked a juvenile court judge to require the teen to continue conventional treatment, and the judge on Friday ordered Abraham to report to a hospital Tuesday. But Accomack County Circuit Court Judge Glen A. Tyler suspended the judge's order. . . . Tyler [also] agreed to a stay and set a trial date of Aug. 16 [and] ended joint custody of Abraham between his parents and social services officials.
In a similar case last year, the parents of 13-year-old Hodgkin's disease patient Katie Wernecke won the right in November to make all her medical decisions after a court fight with Texas child welfare officials. Doctors had recommended chemotherapy and radiation; her father favored a program of intravenous vitamin C.
The 'Net is ablaze with coverage of this story, as well as commentary. Here is a sampling:
Art Caplan is one of the few voices in the wilderness who questions the wisdom of letting young Mr. Cherrix decide his fate:
 While we're talking about patient and family perceptions of end-of-life care in the hospital -- we were talking about that, weren't we? just yesterday? -- Pamela Winnick's essay in the Wall Street Journal on July 21 is well worth considering. She talks about a resident nicknamed "Dr. Death" who pursues family members down the hall to harangue them about her father's alleged desire to be allowed to die a dignified death. She continues:
While we're talking about patient and family perceptions of end-of-life care in the hospital -- we were talking about that, weren't we? just yesterday? -- Pamela Winnick's essay in the Wall Street Journal on July 21 is well worth considering. She talks about a resident nicknamed "Dr. Death" who pursues family members down the hall to harangue them about her father's alleged desire to be allowed to die a dignified death. She continues:This a good reminder for all of us who work with ethics committees and through them with the families of (apparently) dying patients: The "death with dignity" mantra needs to be applied cautiously, patiently, and with sensitivity and a healthy dose of humility."Dr. Death" was just one of several. A new resident appeared the next day, this one a bit more diplomatic but again urging us to allow my father to "die with dignity." And the next day came yet another, who opened with the words, "We're getting mixed messages from your family," before I shut him up. I've written extensively about practice of bioethics -- which, for the most part, I do not find especially ethical -- but never did I dream that our moral compass had gone this far askew. My father, 85, was heading ineluctably toward death. Though unconscious, his brain, as far as anyone could tell, had not been touched by either the cancer or the blood clot. He was not in a persistent vegetative state" (itself a phrase subject to broad interpretation), that magic point at which family members are required to pull the plug -- or risk the accusation that they are right-wing Christians.
I complained about all the death-with-dignity pressure to my father's doctor, an Orthodox Jew, who said that his religion forbids the termination of care but that he would be perfectly willing to "look the other way" if we wanted my father to die. We didn't. Then a light bulb went off in my head. We could devise a strategy to fend off the death-happy residents: We would tell them we were Orthodox Jews.
"My little ruse," she reports, "worked. During the few days after I announced this faux fact, it was as though an invisible fence had been drawn around my mother, my sister and me. No one dared mutter that hateful phrase 'death with dignity.'" Eventually her father was well enough to be transferred out of the ICU and then out of the long-term respiratory care unit. "A day later he was off the respirator, able to breathe on his own. He still mostly slept, but then he began to awaken for minutes at a time, at first groggy, but soon he was as alert (and funny) as ever. A day later, we walked in to find him sitting upright in a chair, reading the New York Times."
 The closing probably won't be till the 4th quarter, assuming the federal regulators bless it and the board doesn't get a better offer, but HCA's board has approved the sale of the company to an aglomeration of investment bankers and the founding Frist family. Of course, no one can quite agree whether the deal is worth $21 billion, $31 billion, or $33 billion, but what's a few billion here or there?
The closing probably won't be till the 4th quarter, assuming the federal regulators bless it and the board doesn't get a better offer, but HCA's board has approved the sale of the company to an aglomeration of investment bankers and the founding Frist family. Of course, no one can quite agree whether the deal is worth $21 billion, $31 billion, or $33 billion, but what's a few billion here or there?The biggest disparity in the reported figures is probably attributable to the $10.6 billion of debt that's being assumed. Once the reporting settles on the value of the deal, it will be in the $31-33 billion range. As Forbes is reporting, their estimate of $31.6 billion would make this the largest leveraged buyout in U.S. history, exceeding KKR's $31.1 billion purchase of RJR Nabisco in 1989. (KKR is also involved in the HCA deal.)
From a health policy perspective, I expect the pundits to ask the question whether for-profit health care ought to be so profitable that it would lead savvy business people to shell out this kind of money. Forbes' title for one of its on-line stories this morning unintentionally sums it up nicely: "Health Is Wealth." When a health care provider can throw of this amount of wealth for private investors, it's bound to fuel questions about whether patients and payers, including the federal government, are paying too much for what they receive.
The investors are also giving us their take on the long-term future of health care in this country. From Forbes: "Apart from betting that economic conditions in the U.S. will remain stable, the suitors will be hoping that the aging American population continues to prompt higher spending on health care, and that the government eventually resolves the problem of uninsured patients."
 After coming oh so close to closing a deal last weekend, it looks like the board is on the verge of approving a $21 billion deal tonight. As reported by the NY Times, "HCA, the nation’s largest for-profit hospital operator, was close to a deal last night to sell itself to a consortium of private equity investors for about $21 billion, people involved in the talks said. The investors would also take on about $10.6 billion of HCA’s debt, making the deal the largest leveraged buyout in history." For-profit healthcare is looking rosy (or, at a minimum, HCA insiders and some savvy investment bankers think HCA's stock is 'way undervalued by the market).
After coming oh so close to closing a deal last weekend, it looks like the board is on the verge of approving a $21 billion deal tonight. As reported by the NY Times, "HCA, the nation’s largest for-profit hospital operator, was close to a deal last night to sell itself to a consortium of private equity investors for about $21 billion, people involved in the talks said. The investors would also take on about $10.6 billion of HCA’s debt, making the deal the largest leveraged buyout in history." For-profit healthcare is looking rosy (or, at a minimum, HCA insiders and some savvy investment bankers think HCA's stock is 'way undervalued by the market). AP/Yahoo has an article today entitled, "Many see accused New Orleans MD as hero." State AG made much of the fact that both morphine and Versed were found in the the bodies of the four patients whose deaths were the basis for his order to arrest Dr. Pou and the two nurses. Contrary to his assertion that the two drugs together can mean only one thing -- that the health care workers' intent was to produce the patients' death -- "Dr. Daniel Nuss (Dr. Pou's department head at LSU) and other doctors said the morphine and Versed that investigators found in the patients' bodies are commonly given to relieve suffering and anxiety. 'If you didn't find sedatives and analgesics in these people, I would think that was inhumane,' [Dr. Ben] deBoisblanc[, director of critical care at Charity Hospital] said. 'The very fact that you found these drugs means nothing.'"
AP/Yahoo has an article today entitled, "Many see accused New Orleans MD as hero." State AG made much of the fact that both morphine and Versed were found in the the bodies of the four patients whose deaths were the basis for his order to arrest Dr. Pou and the two nurses. Contrary to his assertion that the two drugs together can mean only one thing -- that the health care workers' intent was to produce the patients' death -- "Dr. Daniel Nuss (Dr. Pou's department head at LSU) and other doctors said the morphine and Versed that investigators found in the patients' bodies are commonly given to relieve suffering and anxiety. 'If you didn't find sedatives and analgesics in these people, I would think that was inhumane,' [Dr. Ben] deBoisblanc[, director of critical care at Charity Hospital] said. 'The very fact that you found these drugs means nothing.'"
 NPR's Studio 360 program has a wonderful item this week on Emily Dickinson and her iconic poem, "Because I Could Not Stop For Death." The program is available as an MP3 file here.
NPR's Studio 360 program has a wonderful item this week on Emily Dickinson and her iconic poem, "Because I Could Not Stop For Death." The program is available as an MP3 file here.Because I could not stop for Death –
He kindly stopped for me –
The Carriage held but just Ourselves –
And Immortality.We slowly drove – He knew no haste
And I had put away
My labor and my leisure too,
For His Civility –We passed the School, where Children strove
At Recess – in the Ring –
We passed the Fields of Gazing Grain –
We passed the Setting Sun –Or rather – He passed us –
The Dews drew quivering and chill –
For only Gossamer, my Gown –
My Tippet – only Tulle –We paused before a House that seemed
A Swelling of the Ground –
The Roof was scarcely visible –
The Cornice – in the Ground –Since then – 'tis Centuries – and yet
Feels shorter than the Day
I first surmised the Horses' Heads
Were toward Eternity –courtesy of the Academy of American Poets
 Thanks to Joe Paduda's "Managed Care Matters" for pointing me to this story in the Minneapolis-St. Paul Business Journal about a recent article in Mayo Clinic Proceedings: "Adult Intensive Care Unit Use at the End of Life: A Population-Based Study," by Seferian and Afessa [abstract; full text available in 6 months]. As reported in the business journal:
Thanks to Joe Paduda's "Managed Care Matters" for pointing me to this story in the Minneapolis-St. Paul Business Journal about a recent article in Mayo Clinic Proceedings: "Adult Intensive Care Unit Use at the End of Life: A Population-Based Study," by Seferian and Afessa [abstract; full text available in 6 months]. As reported in the business journal:As Paduda points out, these numbers are consistent with a study led by Dartmouth's John Wennberg. As summarized by NewsTarget.com:Intensive care costs comprise 30 to 40 percent of hospital spending and may continue to grow as the population ages, according to a new Mayo Clinic study. Older people with chronic illnesses have the highest rates of intensive-care-unit (ICU) use at the end of their lives, the study found. The country's aging population has an increased prevalence of chronic diseases, signaling that ICUs may treat more and more people in the years ahead. . . .
The study was set in Olmsted County, home of Rochester-based Mayo Clinic, and looked at 818 residents who were admitted to an ICU in 1998. Of those people, one in five died after having received ICU care in the last six months of life. Patients in the last year of their lives accounted for one-fourth of the ICU days used by county residents.
The Dartmouth Atlas Project studied the records of 4.7 million Medicare enrollees who died from 2000 to 2003 and had at least one of 12 chronic illnesses. The study demonstrates that even within this limited patient population, Medicare could have realized substantia savings — $40 billion or nearly one-third of what it spent for their care over the four years — if all U.S. hospitals practiced at the high-quality/low-cost standard set by the Salt Lake City region.
 Back in the day, the phrase "The American Way of Death" invoked Jessica Mitford's classic expose of the funeral industry. In bioethics and law, however, it has a more immediate connotation. With 80% of all Americans dying in an insitutional setting, what is the meaning of "a good death"? And is it possible to achieve in a hospital? Palliative care services notwithstanding, the standard of care for a dying patient typically leaves a lot to be desired. Just how much is well illustrated in an article in the June 21 issue of JAMA (subscription required): "At Face Value" by Karen Donley-Hayes. In discussing her best friend Ashley's death at 36 of breast cancer, she described a process all to familiar to those of us who hang around hospitals:
Back in the day, the phrase "The American Way of Death" invoked Jessica Mitford's classic expose of the funeral industry. In bioethics and law, however, it has a more immediate connotation. With 80% of all Americans dying in an insitutional setting, what is the meaning of "a good death"? And is it possible to achieve in a hospital? Palliative care services notwithstanding, the standard of care for a dying patient typically leaves a lot to be desired. Just how much is well illustrated in an article in the June 21 issue of JAMA (subscription required): "At Face Value" by Karen Donley-Hayes. In discussing her best friend Ashley's death at 36 of breast cancer, she described a process all to familiar to those of us who hang around hospitals:In Ashley's care (with which I have no quarrel), there was no focus on dying until — reluctantly — she went into hospice two weeks before the end of her life. Fortunately, hospice did give us all some preparation for what was to come, but I recall no substantive discussion with the oncologist, or the nursing staff, or the surgeons about what to expect as Ashley died, how to handle it, and what to do — only discussions about how to fight the cancer, until it was clear that fighting was over. Then, it seemed, the entire oncology department removed itself from the picture; even the pain management center seemed to fall short of helping. No one, no organized section of the medical community, came forward to help in the transition from aggressively treating the cancer to helping the patient die. Hospice stepped up to the plate within the scope of its purview, but the medical community, in retrospect, seemed to have hit a wall, as if their jurisdiction to help Ashley in any way ended when it was clear that she would die.
Ashley liked and respected her physicians, liked the nurses who helped with her chemotherapy; for the year and a half of her illness, these people had become, in a way, a part of her family. They knew her by name, knew about her life, what she did, what she liked, her family. For a while, she saw and talked to them nearly as much as the rest of her family. And suddenly, they were gone. Out of the picture. Part of her past. One nurse came to Ashley's memorial service, a gesture that showed us that Ashley had been important to them too; other than that, I did not see any of the members involved in her medical care again. While they were trying to beat this cancer, to win the battle, they were there en masse. When no more chemotherapy or radiation would be administered, they were gone. Looking back, I see this as a sad departure, almost an abandonment. They were there to help her try to live, but they were not there to help her die. . . .
Ashley's situation was unique, because she had several people in her immediate family and close circle of friends who were able to devote themselves to her during her illness and dying process. As time has passed since her death, and I have studied medical ethics and end-of-life issues, it has become clearer to me that there is a gap in the scope of medical care for terminally ill persons: How does the medical community help people die? Can the physicians who govern the treatment of an illness also embrace the care of the patient and the patient's family in the dying process? The disconnect that happens when the "fight" is over is a disservice to the patient. And it's a disservice to the health care professionals as well. They're out of touch with part of the course of the patient's illness, even if they can't cure the illness.
Ashley was very fortunate in so many ways. But what happens to patients who don't have family and friends with the ability or willingness to help them weather the rigors of treatment, or help them die when and if the time comes? Who supports these patients? Who helps their families and friends, who must try and manage this with little or no training or guidance?
Hospice can be a huge help, but it's still a blunt separation from the medical teams that were treating the patient. The transition in care might be the flick of a light switch, but the transition in terms of spirituality, psychology, acceptance for the patient — or the patient's family — cannot be so simple.
If the act of dying isn't shuttled into the closet, if the medical community could embrace it as a natural part of life, the process could be an easier one on everyone — less frightening, less painful, less lonely and rudderless. Death is ugly, scary, and final. But I doubt that any of us want to die feeling impotent, abandoned, no longer in the embrace of the physicians who cared for us when they hoped we might live. A natural part of death for everyone is grief, anxiety, fear, maybe anger. But it can also be a time of growth and enlightenment.
Ashley wasn't timid about dying. The medical profession shouldn't be either.
 Now that the Louisiana Attorney General has had his day (see my earlier post), the extent of AG Foti's grandstanding is starting to come to light. You'd never know it from his office's press release on this case, but consider the following:
Now that the Louisiana Attorney General has had his day (see my earlier post), the extent of AG Foti's grandstanding is starting to come to light. You'd never know it from his office's press release on this case, but consider the following:There's a good article from the L.A. Times on all this.
 Today's New York Times has an article about the recent arrest and prosecution of Dr. Peter Gleason for promoting use of the drug Xyrem, which is approved by the FDA for the treatment of narcolepsy, for the off-label treatment of depression and pain.
Today's New York Times has an article about the recent arrest and prosecution of Dr. Peter Gleason for promoting use of the drug Xyrem, which is approved by the FDA for the treatment of narcolepsy, for the off-label treatment of depression and pain.
 There was a terrific article in The New York Times this past week on the different approaches taken by the public hospitals in Dallas County (Parkland) and Tarrant County (JPS), separated by about 40 miles and a river and a very different view of their missions. This country isn't close to figuring out a humane and sensible approach to immigrant health care, and the conflicts and contradictions are illustrated well by this story. For my money, the approach of the Parkland CEO, Dr. Ron Anderson, is best: "I don’t want my doctors and nurses to be immigration agents."
There was a terrific article in The New York Times this past week on the different approaches taken by the public hospitals in Dallas County (Parkland) and Tarrant County (JPS), separated by about 40 miles and a river and a very different view of their missions. This country isn't close to figuring out a humane and sensible approach to immigrant health care, and the conflicts and contradictions are illustrated well by this story. For my money, the approach of the Parkland CEO, Dr. Ron Anderson, is best: "I don’t want my doctors and nurses to be immigration agents."
 The House failed to override Pres. Bush's veto of H.R.810 by a vote of 235-193, almost the identical vote when it was originally passed by the House in May. Not exactly earth-shattering news, but I offer it for the sake of closure if nothing else.
The House failed to override Pres. Bush's veto of H.R.810 by a vote of 235-193, almost the identical vote when it was originally passed by the House in May. Not exactly earth-shattering news, but I offer it for the sake of closure if nothing else.
 Everything a reporter might need to know to cover this story intelligently -- and the rest of us will find helpful as well -- has been collected, organized, linkified, synthesized, and analyzed by Al Tompkins at the Poynter Center in last Friday's edition of Al's Morning Meeting. Thanks to AJOB's blog for the tip.
Everything a reporter might need to know to cover this story intelligently -- and the rest of us will find helpful as well -- has been collected, organized, linkified, synthesized, and analyzed by Al Tompkins at the Poynter Center in last Friday's edition of Al's Morning Meeting. Thanks to AJOB's blog for the tip.

The news stories on the president's veto haven't mentioned the other bill that was sent to him for his signature, but now that a transcript of the veto/signing ceremony is available from the White House, I can report that he has signed S.3504, the purpose of which is "to prohibit any person or entity involved in interstate commerce from: (1) soliciting or knowingly acquiring, receiving, or accepting a donation of human fetal tissue knowing that a human pregnancy was deliberately initiated to provide such tissue; or (2) knowingly acquiring, receiving, or accepting tissue or cells obtained from a human embryo or fetus that was gestated in the uterus of a nonhuman animal. Imposes fines and/or imprisonment for violations of this Act." It was introduced about a month ago, had no hearings, and produced no committee reports. The nonexistence of this "problem" was conceded by Congressman Joe Barton at the beginning of the House debate on this bill yesterday:
Cong. Rec. H5345 (July 18, 2006)(emphasis added).I rise today in the strongest possible support of S. 3504, the Fetus Farming Prohibition Act. Every so often, we deal with a subject on this floor that is so ugly that the language almost is unable to qualify and quantify that ugliness. Today is one of those moments. When you know what fetus farming is, words like obnoxious and repugnant seem timid.
As we know, fetus farming is the gruesome idea of creating a human fetus purely for research to harvest its organs. This bill would ban that practice, and we cannot ban it, in my opinion, soon enough. Most scientists today share the belief that human life should not be created just for the purposes of experimentation, or for harvesting the organs of one person to be given to another. The vast majority of scientists in our Nation uphold the ethical and moral principles on which our country forever rests, the inalienable right to life and the inherent value of human life in whatever form it may take.
These scientists are working tirelessly with the knowledge that their efforts are to benefit life, benefit humanity, not to benefit one person for profit at the detriment of another person.
Unfortunately, Mr. Speaker, we have seen clear examples in other countries that some scientists see things somewhat differently.
It is towards these scientists that the pending legislation is directed. Rather than waiting for a horror story to appear on the front pages or allowing for the possibility of scientific advancement taking us down a slippery slope, this bill gives a clear signal that fetus farming in all of its forms will not be tolerated in the
United States, nor will we allow human fetuses or embryos to be bought and sold for research like cattle.
 The AP's Mary Dalrymple reports that President Bush has vetoed H.R.810. Here are his reported remarks:
The AP's Mary Dalrymple reports that President Bush has vetoed H.R.810. Here are his reported remarks:"This bill would support the taking of innocent human life of the hope of finding medical benefits for others. It crosses a moral boundary that our society needs to respect, so I vetoed it," Bush said at a White House event where he was surrounded by 18 families who "adopted" frozen embryos that were not used by other couples, and then used those leftover embryos to have children.
"Each of these children was still adopted while still an embryo and has been blessed with a chance to grow, to grow up in a loving family. These boys and girls are not spare parts," he said.
I suppose you can admire his consistency on this issue, though I am more inclined toward Art Caplan's comment that it's a foolish and uninformed consistency. As for the shameless display of of these 18 kids, no one (1) ever doubted that frozen embryos have the capacity to be implanted in a womb and nurtered to maturity or (2) suggested that children so produced were merely "spare parts." That comment well illustrates the vacuousness of the president's policy. And unless I miss my guess, there isn't a state in the country that allows couples to adopt an embryo. Embryo donation is expressly permitted in a number of states, and many (but not all) have paternity rules for the resulting child, but adoption of an embryo? Outside of the federally-funded Snowflakes program -- which appears to result in a purely private, contractual arrangement -- I don't know of a state that has provided for such adoptions by law.
 Art Caplan is at his best today in his column about Bush's promised veto of H.R.810. Here are the opening and closing paragraphs:
Art Caplan is at his best today in his column about Bush's promised veto of H.R.810. Here are the opening and closing paragraphs:President Bush’s embryonic stem cell policy began with lies and has now ended with one.
Bush reserved his first veto as president for one of the only valuable things this do-almost-nothing Congress has managed to actually get done.
With a flourish of a veto pen that has remained dormant no matter how dopey Congress has been, the Senate bill allowing public funding of embryonic stem cell research has been consigned to the legislative trash can. . . .
With his veto the president has now reaffirmed a policy that never made any sense, garnered no scientific support to speak of, was abandoned by both houses of Congress and the leaders of his own party and, most importantly, got no traction with those most in need of the benefits of the research — patients and their families.
The president has now told doctors, researchers and patients to drop dead. Science policy in the Bush administration is best made in the White House, not by scientists and not by Congress.
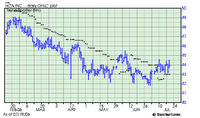 The Wall Street Journal reports (link good for 7 days) that a group of private investors, including members of the founding Frist family, nearly consummated a buyout of HCA over the weekend. With a market capitalization of $17.6 billion, HCA's sale would have been one of the largest in recent memory. It apparently cratered because of the size of HCA's debt ($11 billion), which left the parties about 10% apart on the price. This morning, traders took the attempted buyout as a clear signal that HCA management regards its stock as undervalued in the market. As a result, according to a late-morning story on WSJ_online, HCA's stock price is up 1.5% this morning, while its junk bonds are down sharply.
The Wall Street Journal reports (link good for 7 days) that a group of private investors, including members of the founding Frist family, nearly consummated a buyout of HCA over the weekend. With a market capitalization of $17.6 billion, HCA's sale would have been one of the largest in recent memory. It apparently cratered because of the size of HCA's debt ($11 billion), which left the parties about 10% apart on the price. This morning, traders took the attempted buyout as a clear signal that HCA management regards its stock as undervalued in the market. As a result, according to a late-morning story on WSJ_online, HCA's stock price is up 1.5% this morning, while its junk bonds are down sharply.

 Congress' action on three stem cell bills yesterday and today's expected veto of one of them by President Bush are front-page stories in this morning's Washington Post and New York Times, as was the case in the Dallas Morning News and I suspect most of the dailies around the country. As previously discussed here, this has been a carefully choreographed performance by the Congressional leadership and the White House to give them two fairly meaningless bills (S.2754 and S.3504) the president can sign -- giving the GOP a little defense to play when their Democratic opponents this fall claim the Republicans are against stem-cell research -- as well as another bill (H.R. 810, which would extend federal research support to stem cells derived from leftover IVF embryos) whose veto will allow Republicans to point to their vigilant protection of human life from the moment of conception on.
Congress' action on three stem cell bills yesterday and today's expected veto of one of them by President Bush are front-page stories in this morning's Washington Post and New York Times, as was the case in the Dallas Morning News and I suspect most of the dailies around the country. As previously discussed here, this has been a carefully choreographed performance by the Congressional leadership and the White House to give them two fairly meaningless bills (S.2754 and S.3504) the president can sign -- giving the GOP a little defense to play when their Democratic opponents this fall claim the Republicans are against stem-cell research -- as well as another bill (H.R. 810, which would extend federal research support to stem cells derived from leftover IVF embryos) whose veto will allow Republicans to point to their vigilant protection of human life from the moment of conception on. According to the state's attorney in Louisiana, a physician and two nurses euthanized four patients in LifeCare Hospitals' long-term-care unit at Tenet's 603-bed Memorial Medical Center in New Orleans in the days after Hurricane Katrina devastated that city. (Modern Healthcare). The three were arrested, charged with four counts of second-degree murder, and released on personal recognizance bonds.
According to the state's attorney in Louisiana, a physician and two nurses euthanized four patients in LifeCare Hospitals' long-term-care unit at Tenet's 603-bed Memorial Medical Center in New Orleans in the days after Hurricane Katrina devastated that city. (Modern Healthcare). The three were arrested, charged with four counts of second-degree murder, and released on personal recognizance bonds.Memorial Medical had been cut off by flooding after the Aug. 29 hurricane swamped New Orleans. Power was knocked out in the 317-bed hospital and the temperature inside rose over 100 degrees as the staff tried to tend to patients who waited four days to be evacuated.
In court papers, state investigators said Pou told a nurse executive three days after the hurricane that the patients still awaiting evacuation would probably not survive and that a "decision had been made to administer lethal doses" to them.
Overdoses of morphine or Versed can stop the heart and lungs.
The allegations are that the three administered lethal doses of morphine (a pain killer) and Versed (a sedative). The AP story continues: "Tammie Holley, an attorney for about a dozen families whose relatives died at Memorial, said the presence of the sedative in addition to morphine is important in determining whether the staff members intended to kill. Versed, or midazolam, is used to induce unconsciousness before surgery, according to a medical Web site. 'If it was only morphine, there would be no way to know if they were administering it to control their pain,' Holley said.
Personally, I am inclined to believe that these cases involved attempts to provide pain control and relieve suffering for dying patients who last hours in a hellish environment would otherwise have been wretched. "Double-effect euthanasia" is easy to misinterpret, since so much depends upon the intent of the health-care professional, but there are medical facts that are more or less consistent with an intent to treat, as opposed to an intent to kill, and we will have to know more of those facts before a firm opinion is possible.
The AP story addresses this through Steve Miles:
Dr. Steven Miles, a professor of medicine at the University of Minnesota's bioethics center, said that instead of trying to kill, it is more likely that those charged were trying to relieve patients' pain "in a resource-poor environment and were doing the best they could."
He said that there are documented cases where patients have required seemingly lethal morphine doses to relieve extreme pain, and that he doubts the charges will be proven. "I'm inclined to believe this was palliative sedation that's been misread," Miles said.
Mercy killings would be "not only highly frowned upon, but also rare," Miles said. "It's highly unlikely that's what happened here."
Art Caplan and Steve Miles are also quoted in a later AP story, "Ethicists: No Way to Justify Mercy Deaths" (courtesy of Newsday).
 Andy Stern is president of the Service Employees International Union and in today's Wall Street Journal (link good for at least 7 days), he makes the case for moving health care away from the employer-provided model and toward "a universal system that provides affordable coverage, choice of doctors and insurance plans, core benefits, and shared financing among employers, employees and government." Government leaders won't do the job, Stern writes, so it's up to the CEOs -- "the people who revolutionized medicine, communication, technology, entertainment and investing" -- to provide the leadership on health-care reform.
Andy Stern is president of the Service Employees International Union and in today's Wall Street Journal (link good for at least 7 days), he makes the case for moving health care away from the employer-provided model and toward "a universal system that provides affordable coverage, choice of doctors and insurance plans, core benefits, and shared financing among employers, employees and government." Government leaders won't do the job, Stern writes, so it's up to the CEOs -- "the people who revolutionized medicine, communication, technology, entertainment and investing" -- to provide the leadership on health-care reform.
 The 5 top-downloaded health law articles on SSRN:
The 5 top-downloaded health law articles on SSRN: As reported in this morning's New York Times, U.S. District Judge Fernando J. Gaitan, Jr., previously "had demanded an overhaul of the system after the doctor who now mixes the drugs for the state described an improvised process that Judge Gaitan found so chilling that he temporarily barred executions in Missouri."
As reported in this morning's New York Times, U.S. District Judge Fernando J. Gaitan, Jr., previously "had demanded an overhaul of the system after the doctor who now mixes the drugs for the state described an improvised process that Judge Gaitan found so chilling that he temporarily barred executions in Missouri."The nub of the problem, of course, is that "[t]he American Society of Anesthesiologists and the American Medical Association [Op. E-2.06] say physicians should not take part in executions, and Orin F. Guidry, the president of the A.S.A., recently issued a letter to members reiterating that position in light of the Missouri ruling." Dr. Guidry's description of the ASA position on physician participation is a little more nuanced than The Times lets on, but the ASA apparently comes out the same place as the AMA: "ASA does not have a detailed position on anesthesiologist participation in lethal injection but the 2001 House of Delegates 'Approved a recommendation that ASA support the American Medical Association’s position regarding physician nonparticipation in executions.' . . . . Clearly an anesthesiologist complying with the Missouri ruling – and despite this court’s position on ethical obligations - would be violating the AMA position which ASA has adopted. It is my belief that the court cannot modify physicians’ ethical principles to meet its needs."In a sworn deposition, the Missouri doctor, whose name is being withheld by the state, acknowledged that he had sometimes given the condemned a smaller dose of anesthesia — used to reduce the pain of the lethal drugs to come — than the state had said was its policy.
The doctor said he was solely responsible for counting out dosage amounts of the three drugs administered in sequence, knew of no written protocol by the state for carrying out executions and was at times “improvising.”
He also said he is dyslexic, sometimes mixing up phone numbers or cable bill account numbers. “So it’s not unusual for me to make mistakes,” the doctor, identified in court records as John Doe I, said.
He indicated in his testimony, however, that he had made no mistakes in his death chamber work and that the mistakes elsewhere were “not medically crucial.”
Judge Gaitan said he was “gravely concerned” about the doctor’s dyslexia and criticized the lack of “checks and balances,” ruling on June 26 that the state was subjecting the condemned to “an unnecessary risk that they will be subject to unconstitutional pain and suffering when the lethal injection drugs are administered.”
The judge ordered Missouri to hire a board-certified anesthesiologist (John Doe I is a surgeon), and gave the state until today to submit a formal, written set of procedures, including increased monitoring of inmates and an assurance of sufficient anesthetic drugs.
But in the state’s filing last night, officials said they had sent letters to 298 certified anesthesiologists who reside anywhere near the state’s death chamber in Bonne Terre, and were turned down by all of them.
We are being reluctantly placed on a slippery slope. If the courts demand that inmates be sufficiently anesthetized, then I would have to agree with the court that the only way to assure that would be to have an anesthesiologist prepare and administer the drugs, carefully observe the inmate and all pertinent monitors, and finally to integrate all this information. I don’t think that any of us would want to say that untrained individuals under current death chamber conditions can reliably produce a satisfactory level of unconsciousness. Our core skill is that we can induce an appropriate level of anesthesia. Are we willing to say that untrained individuals can also do so with a reasonable degree of success?
However if the only way to accomplish this appropriate level of anesthesia is with an anesthesiologist using all of our tools AND anesthesiologists will not participate, then are anesthesiologists stopping capital punishment and making public policy?
Not in my opinion. Lethal injection was not anesthesiology’s idea. American society decided to have capital punishment as part of our legal system and to carry it out with lethal injection. The fact that problems are surfacing is not our dilemma. The legal system has painted itself into this corner and it is not our obligation to get it out.
 That's the question raised by a recent request for an Attorney General's Opinion (RQ-0501-GA). The literal question posed by David Swinford (R) (chair of the House Committee on State Affairs) is a bit more technical than that, of course:
That's the question raised by a recent request for an Attorney General's Opinion (RQ-0501-GA). The literal question posed by David Swinford (R) (chair of the House Committee on State Affairs) is a bit more technical than that, of course:Does a physician’s failure to comply with the requirements of either § 164.052(a)(18) (restricting third-trimester abortions performed on viable unborn children) or § 164.052(a)(19) (requiring parental consent for abortions performed on unemancipated minors) of the Texas Occupations Code, as provided by § 1.42 of S.B. 419 (2005 TEX. GEN. LAWS ch 269, § 1.42) subject the physician to liability under the criminal homicide provisions of ch. 19 of the Penal Code?
The analysis says that because it is illegal both for abortions to be performed on a minor without the consent of a parent or guardian and for a physician to perform a third-trimester abortion, doctors who perform them could be prosecuted for murder. The analysis -- written by Shannon Edmonds, the group's director of governmental relations -- says, "This was undoubtedly an unintended consequence but one that law enforcement authorities should be aware of." Edmonds, who said he is unaware of any such prosecutions, said, "After every (legislative) session, there are changes in the law that are real head-scratchers, some intentional and some are unintentional. ... This is just a way to illustrate how unintentional consequences can result in something extreme" (Embry, Austin American-Statesman, 7/13). Swinford, who disagrees with the interpretation of the law by the TDCAA, said the law is intended to provide
criminal penalties for the failure of physicians to obtain parental consent or to comply with restrictions on abortions conducted at or after 28 weeks' gestation, but "certainly not to subject a physician to prosecution for capital murder."
 Excellence in end-of-life care and pain management are also sometimes rewarded by others, in this case by the AHA, which recently gave nurse practitioner Peg Nelson and St. Joseph Mercy Hospital in Pontiac, MI, its Circle of Life Award (which includes $10,000). This article from the Detroit Free Press has the details of their approach to end-of-life care.
Excellence in end-of-life care and pain management are also sometimes rewarded by others, in this case by the AHA, which recently gave nurse practitioner Peg Nelson and St. Joseph Mercy Hospital in Pontiac, MI, its Circle of Life Award (which includes $10,000). This article from the Detroit Free Press has the details of their approach to end-of-life care.
 On Tuesday, the Senate approved (68-32) S. Amdmt. 4548 to H.R. 5441 (Department of Homeland Security Appropriations Act, 2007): "To prohibit the United States Customs and Border Protection from preventing an individual not in the business of importing a prescription drug from importing an FDA-approved prescription drug." As reported by The New York Times on Wednesday, the House is unlikely to get a chance to vote on the Senate's amendment: "[A]ides said that as in past years, the provision was likely to be removed when the legislation got to a conference committee of House and Senate lawmakers who will negotiate the final version."
On Tuesday, the Senate approved (68-32) S. Amdmt. 4548 to H.R. 5441 (Department of Homeland Security Appropriations Act, 2007): "To prohibit the United States Customs and Border Protection from preventing an individual not in the business of importing a prescription drug from importing an FDA-approved prescription drug." As reported by The New York Times on Wednesday, the House is unlikely to get a chance to vote on the Senate's amendment: "[A]ides said that as in past years, the provision was likely to be removed when the legislation got to a conference committee of House and Senate lawmakers who will negotiate the final version." From today's CDC Public Health Law News:
From today's CDC Public Health Law News:"City unveils a plan to identify, and contain, a flu pandemic" -- The New York Times (07/11/06) Diane Cardwell [link]
New York City Mayor Michael R. Bloomberg and city health commissioner Thomas R. Frieden this week announced a new plan to address avian influenza preparedness. The plan details the steps for identifying and containing an outbreak and distributing scarce resources such as antiviral medications. "The fact that New York is a major gateway to the nation and one of the world's most densely populated cities means the possibility of pandemic flu, however remote, is one that we must take extremely seriously," said Bloomberg. The plan stresses early detection to help contain the pandemic, so health officials have taken steps to strengthen communication with doctors and to monitor information about ambulance runs, pharmacy sales, and emergency room visits. In the event of an outbreak, in which the city estimates more than 2.5 million New Yorkers could be infected, officials said they would use traditional methods of containing the virus by encouraging certain behaviors among the public. "It's low technology, but it works: covering your mouth when you cough or sneeze; not going out if you have fever and cough. These are very important things people can do to reduce the spread of infection, and if there were a pandemic, they would be our first line of defense," said Frieden.
[Editor's note: To read the New York City Pandemic Influenza Preparedness and Response Plan, click here.]
 Laurie Kellman of The Washington Post has the story on the upcoming Senate vote on three stem-cell research bills, which were first discussed here two weeks ago:
Laurie Kellman of The Washington Post has the story on the upcoming Senate vote on three stem-cell research bills, which were first discussed here two weeks ago:The Senate will vote next week on three bills related to stem-cell research, including a measure that would expand federal funding for a procedure that uses and destroys human embryos in the drive to cure diseases that afflict millions of Americans [H.R. 810].
The Senate is expected to pass that bill, which would send it to the White House for President Bush's signature. Bush has promised to veto the measure, effectively killing it because neither chamber of Congress has displayed the two-thirds majority needed to override it.
That would be the end of the story, a victory for social conservatives, but for two issues: The Senate debate set to open Monday occurs late in a year of midterm elections, and polls show 70 percent of Americans support the embryonic stem cell bill.
So Senate Majority Leader Bill Frist, R-Tenn., who supports the bill and has spent a year trying to bring it to the floor, succeeded last week by promising opponents to also hold votes on two other stem cell measures they could support and Bush could sign [S.2754 and S.3504].
In a delicate election-year balancing act, Frist also will bring up a measure that would ban so-called "fetal farming," described as growing fetuses for the sole purpose of harvesting tissue. The other would fund research for stem cells derived from adults.
The House would then act quickly to pass the two non-controversial bills and all three would be sent to Bush for his signature. Bush would veto the embryonic bill and sign one or both of the others, giving him and social conservatives in Congress fresh evidence to present to voters this fall that they support stem cell research.
 The current issue of Health Affairs is dedicated to public health. There are some terrific articles, but I particularly commend these:
The current issue of Health Affairs is dedicated to public health. There are some terrific articles, but I particularly commend these: As reported by the Associated Press, New Hampshire judge Edward Fitzgerald "has ordered the state Board of Medicine to stop disciplinary proceedings against a doctor accused of telling a patient she was so obese she might only be attractive to black men and advising another to shoot herself following brain surgery." The article reports that Terry Bennett, M.D., says "he planned to sue everyone involved for 'malicious prosecution.'
As reported by the Associated Press, New Hampshire judge Edward Fitzgerald "has ordered the state Board of Medicine to stop disciplinary proceedings against a doctor accused of telling a patient she was so obese she might only be attractive to black men and advising another to shoot herself following brain surgery." The article reports that Terry Bennett, M.D., says "he planned to sue everyone involved for 'malicious prosecution.' Terrific story (via Kaiser Family Foundation's Daily Health Policy Report) about hospice:
Terrific story (via Kaiser Family Foundation's Daily Health Policy Report) about hospice:McClatchy Newspapers/St. Paul Pioneer Press on Wednesday examined how some patients who check into hospices believing they are near death later go on to recover and leave hospice care. For Medicaid and Medicare beneficiaries to cover hospice care, the patient's doctor and the hospice's doctor must agree that the patient will die within six months. About two-thirds of hospice patients die within 30 days, according to the National Center for Health Statistics at CDC. If a patient does survive six months but is not likely to survive another six months, the patient remains in hospice. Patients who survive six months are discharged if their condition has improved and stabilized enough that they are likely to live another six months. According to CDC data, an estimated 100,000 hospice patients will leave hospice care this year. One study estimates that about one-third of those who leave hospice die within six months of their release. About 5,000 to 20,000 hospice survivors annually "live on with evident satisfaction," while the remainder is transferred to nursing homes, according to McClatchy/Pioneer Press.
Explanation
Experts say there are several factors that can lead terminally ill patients to recover enough to leave hospice care. In many cases, doctors inaccurately estimated how long a patient had to live, McClatchy/Pioneer Press reports. According to McClatchy/Pioneer Press, predicting how long a hospice patient will live might be more difficult today than it was in the 1970s and 1980s, when
three-quarters of hospice patients were admitted because of cancer. By contrast, nearly half of current hospice patients have dementia or heart, lung, kidney or liver failure -- which can make the length of a patient's decline less predictable. "Another theory ... is that pending death brings out the curative power of family and friends," McClatchy/Pioneer Press reports. In addition, some experts say patients might improve in hospice because they are receiving better care than before they entered facilities (Greve, McClatchy/St. Paul Pioneer Press, 7/5).
The article doesn't mention the ill-fated trial balloon from CMS a few years back, in which they proposed to recoup hospice benefits paid to Medicare beneficiaries who didn't die within 6 months!
Also: If you have trouble with the link provided above to the news article (I did!), try this one. Free registration may still be required, but at least the article (eventually) appears on your screen. . . .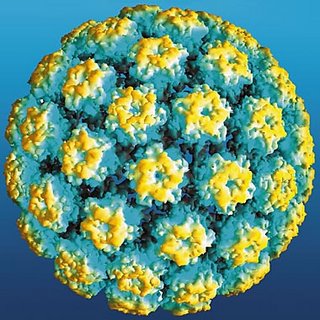 On June 30 Stateline.org published a useful summary of the issues surrounding the recently recommendation from the CDC's Advisory Committee on Immunization Practices that all 11- and 12-year-old girls receive the vaccine for the most dangerous strains of human papillomavirus (HPV), which causes cervical cancer. As a public health matter, the advisory committee's recommendation is pretty straightforward. But the politics of abortion, always lurking just below the surface of any discussion of public policy and sex, promise to alter the debate in many states:
On June 30 Stateline.org published a useful summary of the issues surrounding the recently recommendation from the CDC's Advisory Committee on Immunization Practices that all 11- and 12-year-old girls receive the vaccine for the most dangerous strains of human papillomavirus (HPV), which causes cervical cancer. As a public health matter, the advisory committee's recommendation is pretty straightforward. But the politics of abortion, always lurking just below the surface of any discussion of public policy and sex, promise to alter the debate in many states:. . . HPV is a sexually transmitted disease. The distinction already is spurring some conservative groups to say states shouldn’t mandate that girls get the vaccine, because the only way to catch the cancer-causing disease is through sexual contact.
Linda Klepacki, an analyst on sexual health for Focus on the Family, which promotes abstinence until marriage, said the reason for inoculating schoolchildren for diseases like measles doesn’t apply to the cervical cancer vaccine.
“HPV cannot be communicated by sitting in a public school classroom. It’s communicated only by sexual behavior. Because of that reason, we believe that parents should be the primary decision makers. . . . It’s not something you can catch, but it’s something you really have to go out and get,” she said.
Klepacki acknowledged that women who remain celibate until marriage still could be at risk, if their husbands contracted the virus earlier.
 There's an excellent (and free) article on Roe and partial-birth abortion in this week's New England Journal of Medicine. The authors leave no room for doubt as to their position on legal abortions, including late-term procedures, but their article is no more polemic: it's reasoned and supported by data and careful argument, ending with these four paragraphs:
There's an excellent (and free) article on Roe and partial-birth abortion in this week's New England Journal of Medicine. The authors leave no room for doubt as to their position on legal abortions, including late-term procedures, but their article is no more polemic: it's reasoned and supported by data and careful argument, ending with these four paragraphs:Watson Bowes, emeritus professor of obstetrics and gynecology at the University of North Carolina, is among those who argue that Roe v. Wade is a misuse of federal authority: "The Supreme Court used raw judicial power to trump state legislators, and the decision should be overturned on those grounds." Other antiabortion activists advocate incremental changes in state laws to limit the provision of abortion. These changes include parental consent laws, fetal homicide laws (making it two crimes to kill a pregnant woman), strict regulations for abortion clinics, and legislation requiring physicians to offer women fetal ultrasonography before an abortion.
This strategy is already having an effect, argued Katherine Grainger, legislative counsel at the Center for Reproductive Rights. "With each year, more and more restrictions on Roe are being passed." Ultimately, Grainger said, "we'll see it slowly eviscerated to the point where . . . it's hollow."
Many older abortion providers believe that the complacency of younger women and physicians is partially responsible for the current state of affairs. "They don't remember the thousands of women who died from septic abortions," argued Edelin. "They don't realize that this is a battle to save women's lives — not a battle for choice."
As new legislation is passed, the courts will hear more cases that challenge Roe, and physicians may increasingly risk their careers and their lives if they choose to provide abortions. With each new decision to limit abortion, more American women lose their access. Whether the Supreme Court ultimately upholds or overturns the Partial-Birth Abortion Ban Act, one thing is certain: poor women in rural America are bearing the brunt of these decisions, and some may pay with their lives.
 An article in today's Wall Street Journal (click here - link should be good for about a week) reports that "Americans should expect to pay more for medical costs whether they are employed or retired, according to two new studies. The reports, by Milliman Inc. and Watson Wyatt Worldwide, show that health-care costs are still rising at a fast pace -- despite slowing from double-digit rates in recent years -- and that businesses expect to curtail or limit retiree medical benefits."
An article in today's Wall Street Journal (click here - link should be good for about a week) reports that "Americans should expect to pay more for medical costs whether they are employed or retired, according to two new studies. The reports, by Milliman Inc. and Watson Wyatt Worldwide, show that health-care costs are still rising at a fast pace -- despite slowing from double-digit rates in recent years -- and that businesses expect to curtail or limit retiree medical benefits."The average annual medical cost for a family of four participating in a preferred provider organization, or PPO, program is up 9.6% from 2005 to $13,382 in 2006, according to Milliman, a consulting and actuarial firm that released its second annual study Thursday. Unlike other major health-care cost studies, which look at costs in terms of annual premiums or just the employer's share, the Milliman study also factors in employees' costs, including out-of-pocket expenses.
By my reckoning, even though the reported rate of increase is down a bit compared to reent years, it is still about 2.5-3 times the overall rate of inflation. The outlook for retirees is gloomier than for workers:
Bottom line: more cost pressures on consumers of health-care services. Depending on your politics, this is either a good thing (because it provides an incentive for us to be better, savvier purchasers of health care goods and services) or not (because it pushes increasing numbers of us -- especially those in the worst position to protect themselves (low-income earners and retirees on a fixed income) -- to make tragic choices (drugs vs. food, or Drug A vs. Drug B).The vast majority of businesses are planning to curtail medical plans for current and future retirees, according to the Watson Wyatt study. The survey of 164 companies found that 14% plan to eliminate the benefit for future retirees over age 65, and 6% plan to eliminate it for their current retirees over age 65.
While most employers who still provide the coverage plan to continue it, retirees should expect to pay more for their coverage. "The good news is that they're all not jumping out. The majority are still going to provide it," says Cara Jareb, director of retiree medical consulting at Watson Wyatt. "The bad news is they will be paying more for this coverage."
Nearly two-thirds of employers expect to increase the financial contribution for future retirees, and half expect to change the design of their plans. Twenty-four percent plan to tighten eligibility for future retirees. Fidelity Investments has estimated that a 65-year-old couple retiring without employer-provided health benefits will need $200,000 for out-of-pocket health-care expenses during retirement.
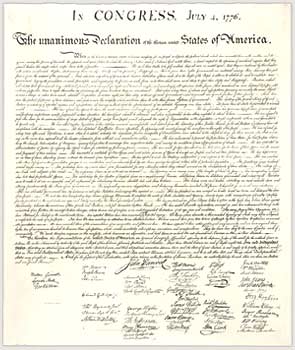 There's something really stirring about listening to the news-readers and commentators on NPR read the Declaration of Independence every 4th of July. If you missed it this morning, click here.
There's something really stirring about listening to the news-readers and commentators on NPR read the Declaration of Independence every 4th of July. If you missed it this morning, click here.