I have a hard time believing the Court will affirm the Fifth Circuit and the District Court and toss out the entire ACA on the specious ground that Congress wouldn't want the ACA to survive without the individual mandate. The premise -- that there is no longer an individual mandate -- flies in the face of the fact that the ACA still contains the individual mandate. The penalty for not purchasing health-insurance coverage was reduced to $0 in the 2017 tax reform law, which renders the mandate a somewhat toothless requirement, But even before 2017, the IRS's collection tools under the ACA were quite limited, which rendered the individual mandate one of the most under-enforced requirements in the United States Code.
Even if the Court agrees that the individual mandate is no more, however, the idea that the Court would go along with tossing out the entire ACA is mind-boggling. That would mean:
- no more prohibition against pre-existing condition exclusions
- no more prohibition against arbitrary and discriminatory rescissions
- no more family coverage for children up to age 26
- the reintroduction of annual and lifetime caps on coverage
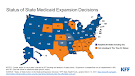
- no more Medicaid expansion funds (raising a serious question about the status of funds for the 39 states that have expanded eligibility based on a promise of a generous (read: massive) federal subsidy)
- the elimination of federal insurance exchanges and possibly state exchanges, too
- the elimination of premium tax credits for low-income households
- the elimination of subsidies for out-of-pocket expenditures
- the elimination of what amounts to a cap on the amount insurers can spend on items other than health-care claims (accompanied by a premium rebate when non-health-care expenditures exceed the permitted amount)
- and on and on and on.