- The doses were about to be destroyed due to nonuse and aging.
- It was his duty as a physician -- and one employed by the Harris County health department -- to maximize health and protect life.
- Allowing the doses to be destroyed would have been a violation of his professional duties and sacred oath.
Health care law (including regulatory and compliance issues, public health law, medical ethics, and life sciences), with digressions into constitutional law, statutory interpretation, poetry, and other things that matter
Thursday, July 01, 2021
Grand Jury Declines to Indict Houston Doctor Accused of Stealing COVID Vaccine
Tuesday, June 29, 2021
Hospitals Now Employ 50% of all U.S. Physicians
Once upon a time, it was a virtually universal no-no for a corporation or other lay entity or person to own, or even have an ownership interest in, a physician's practice. There were various rationales for the so-called "corporate practice prohibition," including:
- only natural persons could meet the requirements for medical licensure,which ruled out corporations, trusts, partnerships, etc.
- a corporate or other lay owner created at least the potential for dual loyalties, putting doctors in the impossible position of choosing between his or her patient and corporate overlords; and
- allowing non-physicians to get in on a medical practice's action represented an unseemly commercialization of medical practice.
Thursday, June 17, 2021
SCOTUS Rejects Red States' Challenge to ACA
In a 7-2 decision (majority opinion by Justice Breyer, dissent by Justice Alito), the Supreme Court today tossed out the suit filed by Texas plus other states and two individuals, not on the merits but for lack of standing.
Basic standing analysis requires a direct harm to the plaintiff that is [1] traceable to an unlawful action or provision of law and is [2] redressable if a court were to give the plaintiff the relief it seeks. The majority opinion concluded that -- even if it agreed that the individual mandate lost its constitutional moorings when in 2017 Congress zeroed out the tax for noncompliance -- the only burdens (i.e., "harms") the plaintiffs could point to were the costs of complying with the presumptively lawful parts of the ACA that remained on the books. It is hard to see how future plaintiffs would be able to overcome the standing hurdle created by this opinion.
As the dissent points out,
Today’s decision is the third installment in our epic Affordable Care Act trilogy, and it follows the same pattern as installments one and two. In all three episodes, with the Affordable Care Act facing a serious threat, the Court has pulled off an improbable rescue.
None of this is to say that challenges to the ACA on other grounds can't or won't be brought, but opponents are running out of constitutional theories. Indeed, the Court has already granted cert. in two ACA cases for the 2021 Term (Nos. 20-429 and 20-539), and there are 6 more ACA cases listed for the Court's next conference. See Nos. 20-219, 20-1162, 20-1200, 20-1374, 20-1432, and 20-1536. All 8 cases are statutory-interpretation cases and none challenge the constitutionality of the ACA or any part of it.
Wednesday, June 16, 2021
Surprise billing: It's still a thing
From the Kaiser Family Foundation's news service:
In Alleged Health Care ‘Money Grab,’ Nation’s Largest Hospital Chain Cashes In on Trauma Centers
After falling from a ladder and cutting his arm, Ed Knight said, he found himself at Richmond, Virginia’s Chippenham Hospital surrounded by nearly a dozen doctors, nurses and technicians — its crack “trauma team” charged with saving the most badly hurt victims of accidents and assaults. But Knight’s wound, while requiring about 30 stitches, wasn’t life-threatening. Hospital records called it “mild.” Nevertheless, Chippenham, owned by for-profit chain HCA Healthcare, included a $17,000 trauma team “activation” fee on Knight’s bill, which totaled $52,238 and included three CT scans billed at $14,000. His care should have cost closer to $3,500 total, according to a claims consultant which analyzed the charges for KHN. (KHN, Richmond Times-Dispatch)
The federal No Surprises Act (signed Dec. 27, 2020) was supposed to curb billing abuses. The KHN link has an exhaustive analysis of the problem, but it doesn't say whether Mr. Knight's trip to the ER was before or after the effective date of the new law. (And the Richmond Times-Dispatch link didn't work for me; I've included it here in case it works for you.)
Monday, June 14, 2021
Public Health: The Neglected Infrastructure Crisis
Dr. Anne Schuchat's June 10th NY Times op-ed is a must-read for any and all who want to understand the importance of investment in public health resources as part of our renewed interest in rebuilding the nation's infrastructure. Published upon the eve of her retirement as second-in-command at the CDC after 33 years of public service. It's a great essay that celebrates public service as a career path. It's also a scary-as-hell depiction of the sorry state of public health in this country. Here's an example:
The Covid-19 pandemic is not the first time the U.S. public health system has had to surge well beyond its capacity, but with the worst pandemic in a century and, initially, a heavily partisan political context, the virus collided with a system suffering from decades of underinvestment. A recent report from the National Academy of Medicine revealed that state and local public health departments have lost an estimated 66,000 jobs since around 2008. [emphasis added]
We cannot count on a once-in-a-century cycle of pandemics. There is every reason to believe that all countries -- the more economically developed chief among them -- are susceptible to increasingly frequent outbreaks.
It's time to wake up and get prepared for when not if.
Wednesday, May 26, 2021
SCOTUS still has to decide a big ACA case
I have a hard time believing the Court will affirm the Fifth Circuit and the District Court and toss out the entire ACA on the specious ground that Congress wouldn't want the ACA to survive without the individual mandate. The premise -- that there is no longer an individual mandate -- flies in the face of the fact that the ACA still contains the individual mandate. The penalty for not purchasing health-insurance coverage was reduced to $0 in the 2017 tax reform law, which renders the mandate a somewhat toothless requirement, But even before 2017, the IRS's collection tools under the ACA were quite limited, which rendered the individual mandate one of the most under-enforced requirements in the United States Code.
Even if the Court agrees that the individual mandate is no more, however, the idea that the Court would go along with tossing out the entire ACA is mind-boggling. That would mean:
- no more prohibition against pre-existing condition exclusions
- no more prohibition against arbitrary and discriminatory rescissions
- no more family coverage for children up to age 26
- the reintroduction of annual and lifetime caps on coverage
- no more Medicaid expansion funds (raising a serious question about the status of funds for the 39 states that have expanded eligibility based on a promise of a generous (read: massive) federal subsidy)
- the elimination of federal insurance exchanges and possibly state exchanges, too
- the elimination of premium tax credits for low-income households
- the elimination of subsidies for out-of-pocket expenditures
- the elimination of what amounts to a cap on the amount insurers can spend on items other than health-care claims (accompanied by a premium rebate when non-health-care expenditures exceed the permitted amount)
- and on and on and on.
Tuesday, May 25, 2021
COVID-19 at the Intersection of Criminal Justice Reform and Public Health
As jails and prisons remain leading sites of COVID-19 outbreaks, mass incarceration poses ongoing health risks for communities. We investigate whether short-term jailing of individuals prior to release may drive COVID-19 spread. We find that cycling individuals through Cook County Jail in March 2020 alone can account for 13% of all COVID-19 cases and 21% of racial COVID-19 disparities in Chicago as of early August. We conclude that detention for alleged offenses that can be safely managed without incarceration is likely harming public safety and driving racial health disparities. These findings reinforce consensus among public health experts that large-scale decarceration should be implemented to protect incarcerated people, mitigate disease spread and racial disparities, and improve biosecurity and pandemic preparedness.
The full article is well worth a close read.
Monday, May 24, 2021
Texas Blows it Again on Medicaid Expansion
Health Affairs has posted a nice summary of the Biden Administration's attempt to entice the hold-out states to expand Medicaid pursuant to the ACA (though it unfortunately has absolutely no relevance to Texas -- read on):
In the newest addition to our “Eye On Health Reform” series, Katie Keith covers the American Rescue Plan Act, which was signed into law by President Joe Biden in March.
Keith explains that the legislation temporarily expands the Affordable Care Act’s premium tax credits and increases federal financial incentives for holdout states to expand their Medicaid programs. Keith also explores enrollment trends in states that use HealthCare.gov, current ACA litigation, and ACA guidance from the Biden administration.
I wrote about an earlier plan to pay hold-outs on Feb. 16, back when the prospects for expansion in Texas seemed, if not bright, at least alive. By my count there were five House bills, two Senate bills, four House Joint Resolutions, and three Senate Joint Resolutions that would have authorized (or required) Texas to take advantage of the federal dollars that would become available if Texas were to expand Medicaid eligibility to 138% of the federal poverty limit. Would it be cynical of me -- or simply realistic -- to report that every single one of these proposals died in committee? Every one! What is there to say other than it really sucks to be poor and live in Texas, where the legislature seems determined to keep a minimum level of health care out of reach for five million of its citizens.
For the record, here are the links to the bills and JRs, along with the names of co-sponsors:
HJR 9, 23, 24, 86
SJR 11, 14, 15
HB 143, 398, 513, 1730, 4406
SB 38, 119
Tuesday, May 11, 2021
"What Has President Biden Done in Health Care Coverage in His First 100 Days?"
Tuesday, March 23, 2021
AstraZeneca in Major Dispute with U.S. Regulators
Late Monday, the Data and Safety Monitoring Board (DSMB) notified NIAID, BARDA, and AstraZeneca that it was concerned by information released by AstraZeneca on initial data from its COVID-19 vaccine clinical trial. The DSMB expressed concern that AstraZeneca may have included outdated information from that trial, which may have provided an incomplete view of the efficacy data. We urge the company to work with the DSMB to review the efficacy data and ensure the most accurate, up-to-date efficacy data be made public as quickly as possible.
It is almost (but not quite) inconceivable that AstraZeneca made an innocent error. The DSMB is accusing the firm of essentially "cherry-picking" the data “most favorable for the study as opposed to the most recent and most complete.” (NY Times, 3/23) The DSMB's letter to the NIH and AstraZeneca stated that the efficacy rate of the firm's COVID-19 vaccine might be between 69% and 74%, rather than the 79% rate touted by AstraZeneca itself. Did AstraZeneca really think they could slip one past the regulators? And at what cost to its reputation? Not to mention at what cost to the worldwide public-health crisis, where mistrust of science and vaccine-skepticism don't need any more encouragement and support.
From the Times article: “'Decisions like this are what erode public trust in the scientific process,' the board wrote."
Monday, March 22, 2021
Medicaid Expansion in Texas: The Time is Now
The Legislature is back in session. A bill has been introduced to authorize Texas to accept the federal government's offer to pay for 90% of the cost of expanding Medicaid eligibility to include all Texans under the age of 65 (when Medicare kicks in) and whose income does not exceed 138% of the federal poverty level: HB 1730, introduced by Republican Representative Lyle Larson. Sen. Johnson's own companion bills are SB 118 and SB 119.
The case for expansion is made in a most compelling and entertaining video (10.5 minutes) by Senator Nathan Johnson (D-Dist. 16 (which covers a big chunk of Dallas)). Please watch it. Share it with your family. Send it to your friends. Get involved. We have already waited too long, left billions of federal dollars on the table, and worst of all, we've ignored the health care needs of 1 million Texans who would benefit from expansion. Let's make this happen this year.
And thanks to DFW Hospital Council CEO Stephen Love for passing the video on to me.
Monday, March 08, 2021
CDC's Guidance for "Fully Vaccinated People"
The guidance was issued earlier today, and you can read the whole document here. Meanwhile, here are the highlights:
Key Points
This is the first set of public health recommendations for fully vaccinated people. This guidance will be updated and expanded based on the level of community spread of SARS-CoV-2, the proportion of the population that is fully vaccinated, and the rapidly evolving science on COVID-19 vaccines.
For the purposes of this guidance, people are considered fully vaccinated for COVID-19 ≥2 weeks after they have received the second dose in a 2-dose series (Pfizer-BioNTech or Moderna), or ≥2 weeks after they have received a single-dose vaccine (Johnson and Johnson [J&J]/Janssen ).†
The following recommendations apply to non-healthcare settings.
Fully vaccinated people can:
Visit with other fully vaccinated people indoors without wearing masks or physical distancing
Visit with unvaccinated people from a single household who are at low risk for severe COVID-19 disease indoors without wearing masks or physical distancing
Refrain from quarantine and testing following a known exposure if asymptomatic
For now, fully vaccinated people should continue to:
Take precautions in public like wearing a well-fitted mask and physical distancing
Wear masks, practice physical distancing, and adhere to other prevention measures when visiting with unvaccinated people who are at increased risk for severe COVID-19 disease or who have an unvaccinated household member who is at increased risk for severe COVID-19 disease
Wear masks, maintain physical distance, and practice other prevention measures when visiting with unvaccinated people from multiple households
Avoid medium- and large-sized in-person gatherings
Get tested if experiencing COVID-19 symptoms
Follow guidance issued by individual employers
Follow CDC and health department travel requirements and recommendations
Thursday, March 04, 2021
Free Webinar: Pres. Biden's First 100 Days of Health Policy
Boston University's Center for Health Law, Ethics & Human Rights faculty discuss the first 100 days of President Biden’s term:
- Executive Orders,
- proposed bills, and
- other steps to tackle COVID, climate, and economic crises affecting health.
1:00 - 2:30 p.m. EST
SPEAKERS
George Annas
Nicole Huberfeld
Wendy Mariner
Michael Ulrich
JOIN ZOOM MEETING
https://bostonu.zoom.us/j/93372687004?pwd=NXpoNm5wZW1YOEljeENyeWY2V3dVUT09
Meeting ID: 933 7268 7004
Passcode: 331167
Tuesday, March 02, 2021
"Governor Abbott Lifts Mask Mandate, Opens Texas 100 Percent" [source: Governor's website]
Yes, it's true. Governor Abbott (along with the Governor of Mississippi) has earned the title "Worst Public Health Decision Maker Still Holding Office in the U.S." with this announcement. The full text of Executive Order GA-34 is here.
Gov. Abbott offered remarks on his remarkable EO in Lubbock. Here is an annotated paragraph:
"With the medical advancements of vaccines and antibody therapeutic drugs, Texas now has the tools to protect Texans from the virus,” said Governor Abbott.
You bet we have the tools. We simply have to use them.
"Make no mistake, COVID-19 has not disappeared, but it is clear from the recoveries, vaccinations, reduced hospitalizations, and safe practices that Texans are using that state mandates are no longer needed."
Wow, that's a whopper. To borrow a line from Justice Ginsburg's dissent in Shelby County, in which the majority held that the Voting Rights Act's preclearance mechanism was no longer needed: "Throwing out preclearance when it has worked and is continuing to work to stop discriminatory changes is like throwing away your umbrella in a rainstorm because you are not getting wet." [Opinion, p. 33]
"Today's announcement does not abandon safe practices that Texans have mastered over the past year."
Another whopper. Texans haven't mastered safe practices and now we've been given a green light to abandon them altogether.
"Effective next Wednesday [Mar. 10], all businesses of any type may open to 100% capacity." "This order ends the statewide mask mandate in Texas."
Abbott helpfully notes that anyone who wants to can wear a mask and businesses can self-limit their own capacity. That's the kind of right-thinking Texas policy that gave us ERCOT and the disaster of two weeks ago. We are going our own way and celebrating Texas independence. Wonderful spirit, but lots of people died. And lots of people are going to die of COVID-19 unnecessarily because of today's order.
Stephen Love, the President/CEO of the Dallas-Fort Worth Hospital Council had this to say:
"While we respect Governor Greg Abbott and realize he has faced enormous challenges with the COVID-19 pandemic and recent weather issues, we strongly disagree with removing the mandatory mask requirements. This decision will cause the community spread to increase, forcing our exhausted healthcare heroes to diagnose, treat and save the lives of newly infected patients. If the community spread increases, the risk of mutations will also increase, creating a new set of potentially dangerous challenges. If you truly want to honor our healthcare heroes, then continue to wear a mask! We ask Governor Abbott to please reconsider his decision."
Back to the governor:
"Instead, it is a reminder that each person has a role to play in their own personal safety and the safety of others."
Agreed. What the Executive Order ignores is that the state has a role to play, as well. And the governor has just abandoned that responsibility.
"With this executive order, we are ensuring that all businesses and families in Texas have the freedom to determine their own destiny."
And the destiny of all others -- family, workers, strangers -- with whom they come into contact. Gulp.
Sunday, February 21, 2021
COVID-19 Vaccination and Ethics: Stanford/AJOB Webinar
The American Journal of Bioethics and Stanford's Center for Biomedical Ethics (David Magnus & Bela Fishbeyn) on Feb. 16 put on an excellent panel discussion of the ethics of COVID-19 vaccination policies. It was a far-ranging discussion with knowledgeable participants and well worth watching.
Saturday, February 20, 2021
Medicaid in Times of Crisis: A GAO Report (2 pp.)
It's short but sweet. The Government Accountability Office has issued GAO-21-343SP (02-17-2021), a nifty description and analysis of the role of the federal-state Medicaid program in times of crisis (e.g., epidemics and pandemics, economic recessions, natural disasters, and personal health crises). Specific examples over the past 15 years include Hurricane Katrina, the Great Recession, the opioid epidemic, and of course COVID-19.
This is further proof, as if any were needed, that Texas's policy of not expanding Medicaid eligibility at largely federal expense isn't only hurting the indigent (and largely minority) individuals -- including millions of kids -- that legislators seem keen to punish for being, you know, indigent, nonwhite, and young. The policy is also depriving public-health officials of an important tool in times of great public need.
Thursday, February 18, 2021
COVID Vaccine and Health Equity: We have a long way to go
From Kaiser Health News (2/18/2021):
KFF has an updated analysis of state-reported data as of February 16, 2021 on COVID-19 vaccinations, cases, and deaths by race/ethnicity.
New to the analysis are comparisons of vaccination rates in each racial/ethnic group based on state-reported data of total people who have received at least one dose of the vaccine. Among just over half of states reporting data, the vaccination rate among White people is over three times higher than the rate for Hispanic people (10% vs 3%) and twice as high as the rate for Black people (10% vs. 5%). The vaccination rate for Asian people is closer to the rate for White people in most reporting states, although they are less likely to have been vaccinated in most reporting states.
Wednesday, February 17, 2021
Planned Parenthood, Medicaid Expansion, and Women's Health
Another example of weaponization was pointed out in an op-ed in the New York Times (02-17-2021) by Dr. Samuel Dickman, an internist and the medical director for primary care at Planned Parenthood South Texas:
For the past several years, Texas politicians have worked to cut off Medicaid recipients’ access to the wide range of services offered by Planned Parenthood. Now, barring an extension of a state district court’s temporary block on their efforts, they may have gotten their way.
Gov. Greg Abbott, a Republican, and like-minded state officials targeted Planned Parenthood because it offers abortion services. But abortion services account for just a fraction of the care we provide, which means the consequences of a new policy would be far more sweeping.
If it goes into effect, this policy would block patients’ access to blood pressure checks, cancer screenings, birth control, S.T.D. treatment and other medical care routinely provided at Planned Parenthood health centers in Texas, where I serve as a medical director for primary care. Nationally these other essential services, not abortion care, account for 96 percent of Planned Parenthood’s patient visits; in Texas, for example, some 24,000 Medicaid patients received non-abortion care over the past four years.
The aforementioned cruel and punitive nature of the proposed change should be obvious:
States’ denials of health care coverage, including Texas’ refusal to expand Medicaid, contributed to 461,000 excess deaths in 2018 that would have been averted if the United States had kept up with other wealthy countries, a tragedy documented in a report by my colleagues and me published this month in The Lancet.
It is also just bad policy. Not just bad health policy, which it obviously is, but bad fiscal policy as well. Untreated STDs will increase the cost of health care because of expensive later treatments. Forgone cancer screenings, untreated hypertension and a host of other chronic conditions only get more expensive the longer preventive care is postponed denied once Planned Parenthood is knocked out of the Medicaid program altogether. Gov. Abbott and his pals have to be stopped. If they aren't, any Medicaid expansion that Texas may stumble into (see yesterday's post) will leave these 24,000 women and many others in years to come out in the cold.
Tuesday, February 16, 2021
Medicaid Expansion: Biden's COVID Relief Proposal Includes a Cash Sweetener for Texas and 11 Other Holdouts
As reported by The Washington Post (02/16/21), the 5,593-page COVID relief bill supported by the Biden Administration contains a provision to increase Medicaid reimbursements by 5 percent for holdout states that finally do the right thing and expand Medicaid eligibility to 133 percent of the federal poverty line. Some excerpts from the Post's article:
Texas has more uninsured residents than any other state — partly because the massive state has spurned expansion. That means no Medicaid for most adults earning up to 133 percent of the federal poverty level (around $17,000 for a single person or $35,000 for a family of four). . . .
A coronavirus relief bill working its way through Congress and backed by President Biden includes a hefty incentive for states to expand Medicaid. If a state did so, the federal government would increase its Medicaid contribution to the state by 5 percent. The increased match rate would apply to everyone outside the expansion group and would last two years.
For Texas, that would mean nearly $6 billion extra dollars in Medicaid funds over two years. . . .
It appears that a handful of Republican legislators -- and even Governor Abbott -- may be warming to the idea of accepting billions of federal dollars in order to provide decent health care to over 5 million uninsured Texans (that's 17.7% of the population, more than double the national rate of uninsured (8.5%).
This shouldn't even be debatable. But maybe, just maybe, the times (and the state) are a-changin'. San Antonio's Republican Representative Lyle Larson has introduced HB 1730, a bill "[r]elating to the expansion of eligibility for Medicaid to all persons for whom federal matching money is available." Fingers crossed.
Friday, February 12, 2021
Welcome to the Wacky World of Hospital Pricing Practices
When a woman gets a caesarean section at the gleaming new Van Ness location of Sutter Health’s California Pacific Medical Center, the price might be $6,241. Or $29,257. Or $38,264. It could even go as high as $60,584.
Sutter Health isn't doing anything illegal or even unique. It bills different amounts based on whether the patient is uninsured, insured, a subscriber to the Sutter Health HMO, or (worst-case scenario) out-of-network. There is a historical and economics-based rationale for the way serves are priced in the hospital's ChargeMaster and ultimately billed to patients and payers of various stripes. Unfortunately, the history and accounting rationales conspire to hurt the patients least able to protect themselves with health insurance, Health Savings Accounts, and the like. I hope everyone has a chance to read this article.
Thursday, February 11, 2021
Biden Administration Reverses Trump's Position on ACA SCOTUS Litigation
In a two-page letter from the Office of the Solicitor General makes two simple assertions, with which neither the trial court nor 5th Circuit agreed:
- When in 2017 Congress reduced to zero the monetary penalty imposed by the ACA on individuals who failed to secure health insurance coverage (the individual mandate, or the "play or pay" provision), the mandate didn't become unconstitutional by implication. The lawful choice between buying insurance coverage and not buying insurance coverage remained.
- Even if the the Court disagrees with ¶ 1 and strikes down the mandate, the mandate is severable from the rest of the ACA, meaning the other provisions of this massive statute are left in place.
Wednesday, January 27, 2021
"HHS Misused Millions of Dollars Intended for Vaccine Research, Emergency Preparedness" (HHS Special Counsel Report, 1/27/21)
This is distressing, both because the practice of siphoning these funds away from their intended use thwarts the intent of congressional appropriators and because the practice apparently started in the Obama administration. The generic issue of moving funds around from program to program is, of course, much older and more widespread than this one fund and the ten years that its funds have been raided. The first paragraph of the Special Counsel's news release tells the story:
The U.S. Office of Special Counsel (OSC) today sent letters to the President and Congress alerting them that, over the last decade, the U.S. Department of Health and Human Services (HHS) misappropriated millions of dollars Congress intended to fund vaccine research and emergency preparedness for public health threats like Ebola, Zika, and COVID-19. A whistleblower alerted OSC to the misuse of funds appropriated to the Biomedical Advanced Research and Development Authority (BARDA) within HHS. OSC referred the allegations for investigation by the agency, which was conducted by HHS's Office of Inspector General (OIG). The investigation substantiated many of the allegations, finding that since at least fiscal year (FY) 2010, the Office of Assistant Secretary for Preparedness and Response (ASPR) misused funds appropriated for BARDA and failed to accurately report this mismanagement to Congress.
The report contains evidence that ASPR used BARDA's research funds to pay for myriad unrelated expenses, including the removal of office furniture, administrative expenses, news subscriptions, legal services, and the salaries of personnel who did not work for BARDA. The report reveals that the practice of using BARDA funds for non-BARDA purposes was so common, there was even a name for it within the agency: “Bank of BARDA." HHS OIG determined that ASPR had “violated the Purpose Statute" and “potentially violated the Antideficiency Act."
How much money are we talking about here? Potentially a lot (except half a billion dollars in the scheme of the federal budget may not seem like much):
While the report does not contain a specific estimate for total funds misappropriated, it contains evidence that as recently as FY 2019, approximately $25 million was taken from BARDA's Advanced Research and Development (ARD) programs and improperly provided to ASPR. Moreover, from FY 2007 to 2016, ASPR's reporting to Congress failed to account for $517.8 million in administrative expenditures. The report found that “ASPR is unable to demonstrate that the[se] BARDA funds were used for their appropriated purposes."
It is fairly common to move funds from one small program that no one cares that much about to another program that is facing a budget shortfall -- not any less illegal, but it is done. But this raid on the "Band of BARDA" hit the programs -- vaccine development and emergency preparedness -- that are central to the health of the public right now. I think this is a story that isn't going away anytime soon.
Tuesday, January 19, 2021
Beyond the Health Policy "Iron Triangle" of Cost, Quality, and Access"
There's a new article that builds on our experience with pandemic response to make the case for increasing emphasis upon health justice -- equity and public health. "Health Reform Reconstruction" is a free download on SSRN and is well worth the time to read and reflect on its message. Authors Lindsay F. Wiley, (American University - Washington, College of Law), Elizabeth Y. McCuskey (University of Massachusetts School of Law, Center for Health Law Studies), Matthew B. Lawrence (Emory University School of Law, Harvard University - Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics), and Erin C. Fuse Brown (Georgia State University College of Law) provide this Abstract:
This Article connects the failed, inequitable U.S. coronavirus pandemic response to conceptual and structural constraints that have held back U.S health reform for decades – and calls for reconstruction. For more than a half-century, an intellectually cramped “iron triangle” ethos has constrained health reform conceptually. The iron triangle centered individual interests in access to, quality of, and cost of medical care, while marginalizing equity and public health. In the iron triangle era, reforms unquestioningly accommodated four entrenched fixtures of American law—individualism, fiscal fragmentation, privatization, and federalism—that distort and diffuse any reach toward justice and solidarity. The profound racial disparities and public health failures of the U.S. pandemic response in 2020 agonizingly manifested the limitations of pre-2020 health reform and demand a reconstruction.
Health reform reconstruction begins with the replacement of the iron triangle era with a new era in which reforms aim to realize health justice. Health justice does not itself overcome the fixtures of American law that constrain reform and propagate subordination. But it reveals the importance of doing so, despite the fixtures’ stubborn legal and logistical entrenchment. Because health reformers can no longer accept any conceptual goal short of health justice, incremental reforms must be measured chiefly by whether they confront or accommodate individualism, fiscal fragmentation, privatization, and federalism in health care. Through an uncompromising conceptual aspiration and a method of confrontational incrementalism focused on dismantling the legal structures that stand in the way of health justice, health reform reconstruction is possible. The Article describes how health reform reconstruction can chart the path of legal change and reflects on the usefulness of its methodology of confrontational incrementalism in other fields which recognize the necessity of reconstructive reform, along with its near impossibility, such as policing and drug policy.
Expect state and local governments to re-impose more severe restrictions over the next few month
The vaccination program should slow things down, but in addition to vaccine skepticism, the rollout has been agonizingly slow, poorly organized, and far from clearly marketed. Initial shots are supposed to have some effect, but it remains to be seen whether second shots will be available on-schedule. And in any event, masking and social distancing are still called for and will be for the foreseeable future. It's pretty clear that "pandemic fatigue" has set in, so these traditional public-health measures, which have been demonstrated time and again to be effective against the spread of respiratory viruses, are waning in effectiveness.
Finally, there are now at least three mutations of the novel coronavirus that make the disease potentially more contagious than the original form of the virus. They have appeared in the United Kingdom, South Africa, and Brazil. (The Atlantic, 1/18/21) Our own genomic surveillance is pitifully inadequate to provide reliable data, but at least two of the variants (a fixed cluster of mutations, according to virologists) have appeared in this country.
As Dr. Fauci has explained, all of this adds up to a dismal winter season (CNN, 12/27/20) and a not-much-better spring, with growing pressure on governors and regulators to impose restrictions at least as severe as those in place last summer.
Sunday, January 17, 2021
Lana Del Rey's eerie, conspiracy-laden music video and the death of Phil Spector
It's a pretty tune -- "Chemtrails Over the Country Club" -- accompanied by a spooky video with an apocalyptic conclusion to go along with it. The video features occasional flashes of those wispy white tracks produced by the hot vapors emitted by jet engines: "contrails" (short for "condensation trails" (a/k/a "vapor trails")). It turns out contrails contribute significantly to global warming, so they are far from benign in and of themselves. But conspiracy theorists believe the jets are putting out trails of deadly chemicals ("chemtrails") for -- as described by Scientific American -- "a variety of nefarious purposes from weather modification, to human population control via sterilization, to even mind control." Ms. Del Rey is the queen of "heroin chic" and wears her infamous mesh face mask in this video, and if she is anyone's source of scientific information . . . well, I don't suppose they are also readers of Scientific American. This isn't the first nihilistic pop tune to come down the road, to be sure (I am old enough to remember 1965's "Eve of Destruction"), but I am suddenly feeling very, very old. The high point of the video for me was the gorgeous cherry red Mercedes 540 K that she drives until (spoiler alert) she sets it on fire (undoubtedly a replicar, but still a work of art).
Speaking of the dark side of pop culture, Phil Spector died yesterday of COVID-19 while serving a prison sentence for the murder of an aspiring actress in his home in 2003 (NY Times, 1/17/20). He produced some of the most glorious pop and rock of the 1960s and 1970s, but his mind slipped into a very dark place over the next 30 years. Coincidentally, Hal Blaine, the drummer in Spector's heralded studio band, The Wrecking Crew, played on "Eve of Destruction." You can't make this stuff up.
Monday, January 04, 2021
Super-Spreader Events = Not-So-Happy New Year
Thursday, December 31, 2020
Ten Lessons from Health Affairs
The esteemed health-policy journal Health Affairs has published its list of "Ten Lessons from COVID-19 Research Published in Health Affairs" (12/30/20). Number 10 shouldn't have surprised me, but it did:
- Mandating face masks in public is associated with a decline in the daily COVID-19 growth rate.
- COVID-19 emergency sick leave has reduced confirmed cases.
- Increased testing and isolation may be the most effective, least costly alternative—in terms of money, economic growth, and human life—for controlling COVID-19.
- Shelter-in-place orders reduce both daily COVID-19 hospitalizations and mortality growth rates within weeks of enactment.
- Blacks and Hispanics are more likely to screen positive, be hospitalized, and die due to COVID-19 relative to non-Hispanic Whites.
- Vaccine implementation, including the pace of vaccination and the percent of the population ultimately vaccinated, will contribute more to the success of vaccination programs than a vaccine’s efficacy determined in clinical trials.
- Hospitals reinvented patient and staff support systems during the COVID-19 pandemic to better cope with trauma.
- Expanded Medicaid coverage and insurance reimbursement for telehealth played a pivotal role in the rapidly increased use of these services during the pandemic.
- The majority of school employees and school-age children live in households including at least one adult with increased risk for severe COVID-19, and about half of all school employees have increased risk themselves.
- Unionized health care workers in nursing homes were associated with a decrease in COVID-19 mortality rates and greater access to personal protective equipment for workers.
Wednesday, December 30, 2020
What to Expect in Year Two of the Pandemic
Ed Yong is widely regarded as the best journalist on the COVID-19 beat, and he's just published in The Atlantic (1/29/21 (free)) his projections for Year 2 of the current pandemic. This summary barely does justice to the full piece, which is rich in details and supporting references:
1. The vaccine rollout could be rocky.
“We are trying to plan for the most complex vaccination program in human history after a year of complete exhaustion, with a chronically underfunded infrastructure and personnel who are still responsible for measles and sexually transmitted diseases and making sure your water is clean,” [Kelly Moore of Vanderbilt University, who studies immunization policy,] said.
2. The virus could change.
What happens next with SARS-CoV-2 depends on how our immune systems react to the vaccines, and whether the virus evolves in response. Both factors are notoriously hard to predict, because the immune system (as immunologists like to remind people) is very complicated, and evolution (as biologists often note) is cleverer than you.
3. But expect some relief by the summer.
Many of the 30 epidemiologists, physicians, immunologists, sociologists, and historians whom I interviewed for this piece are cautiously optimistic that the U.S. is headed for a better summer. But they emphasized that such a world, though plausible, is not inevitable.
4. Still, this outbreak will leave long-term scars.
A pummeled health-care system will be reeling, short-staffed, and facing new surges of people with long-haul symptoms or mental-health problems. Social gaps that were widened will be further torn apart. Grief will turn into trauma. And a nation that has begun to return to normal will have to decide whether to remember that normal led to this.
National Academy of Medicine Webinar on Crisis Standards of Care
This looks like a good lineup of panelists asking (and I hope answering) the right questions:
As hospitals and other providers experience significant patient surge at a pivotal stage of the COVID-19 pandemic, the National Academy of Medicine and its partners have called on federal, state/territorial, and tribal leaders and private sector actors to shift to crisis standards of care. Resource scarcities of available ICU beds, personnel, treatments, personal protective equipment, and vaccinations justify critical changes in health care delivery. Yet substantial legal and policy issues can stand as obstacles to implementation without real-time solutions.
In this session, Dr. Dan Hanfling, Professor James Hodge, and Research Scholar Jen Piatt will examine key legal issues underlying crisis standards of care. These include
- concerns surrounding emergency declarations,
- invocation,
- duties to care,
- inter-jurisdictional challenges,
- discrimination,
- licensure/scope of practice,
- risks of liability,
- documentation, and
- mitigation.
Potential solutions to real-time issues will be offered, including through direct questions among attendees and others.
Date: 1/7/21
Time: 3:30-4:45pm EST
Registration -- free -- is here.
Tuesday, December 29, 2020
Lawrence Wright in The New Yorker: For now, the definitive history of the novel coronavirus in 2020
Sunday, December 27, 2020
Pres. Obama's Inside Story on the Rocky Road to Obamacare
With "about six in ten of the public say[ing] they or someone in their household suffers from a pre-existing or chronic medical condition, such as asthma, diabetes, or high blood pressure," the most popular provision remains the prohibition against discrimination by health insurers based upon preëxisting conditions. (Kaiser, 12/18/20) And now that the wildly unpopular individual mandate has been rendered completely toothless by the tax reform legislation in 2017, the favorable-over-unfavorable gap in public opinion is 19%, the largest it's been since enactment.
Monday, December 21, 2020
Top 10 Health Stories of 2020: Nearly All Are Healthlaw-Related
From The Commonwealth Fund (more details are here):
- "COVID-19 hits the United States." The greatest public health (and public health law) crisis in a century.
- "Pandemic takes a devastating toll on health." Public health measures alone don't protect against the virus. Compliance matters.
- "Economic fallout." COVID-19 has put pressure on every level of government. Some performed brilliantly, a few failed miserably, and for the rest the report card was mixed.
- "FDA authorizes coronavirus vaccine and distribution begins." A stunningly successful public-private partnership produced unprecedented results, though Pfizer -- the first to get FDA approval -- turned down federal funding.
- "Dramatic leapfrogging in telehealth." Regulators at both the federal and state levels proved to be fairly nimble in providing authorization and reimbursement for greatly expanded telemedicine services. This is probably one of many developments that won't go away after the virus has been controlled. Telemedicine will be part of the "new normal."
- "Racial injustice protests draw attention to health disparities." It's not as if there are plenty of federal and state laws on the books to deal with discrimination in health care, but health disparities remain. There's a lot more work to do on this front.
- "The future of the Affordable Care Act is still unknown." It is, once again, in the hands of SCOTUS. Chief Justice Roberts was the architect (and principal author) of the Court's two previous encounters with potentially ACA-killing litigation. With a revised lineup of Justices, will he provide the saving grace in Texas v. U.S.?
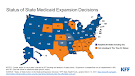
- "Medicaid expansion continues at a slow and steady pace." Three states voted to expand Medicaid eligibility pursuant to the ACA; twelve continue to impede the ACA's promise of expanded coverage at virtually no cost to the states. Texas -- with the largest number and percentage of uninsured citizens in the U.S. -- remains a notable holdout. Consider the billions of federal dollars Texas providers have been denied during the COVID-19 crisis, which has seen provider and after provider, especially in rural areas, close up shop
- "Joe Biden is elected president." We will soon have a resident in the White House who isn't trying to hobble the ACA and cast doubt on the bona fides of public-health authorities at every turn.
- "Biden appoints new health care team." With a few exceptions, the Trump cabinet was filled with amateurs with either no experience or a predisposition to cut back on enforcement of federal programs or both. The new cabinet and sub-cabinet appointees look to reverse the trend.
Friday, December 11, 2020
More on COVID-19 and Employer Mandates and more and more . . .
Morrison & Foerster LLP issued a report on Wednesday, 12/9/20, based on a survey of in-house legal professionals around the world. The top legal concerns that came out of the survey were: employment and labor, data security, and contract disputes.
On the subject of vaccine mandates, the subject of my post yesterday, MoFo concluded: "“With one or more vaccines on the verge of being approved, some employers will undoubtedly mandate employee vaccines, either for altruistic reasons – they don’t want people to get sick at their place of business – or because they are worried about liability for workplace exposure to COVID-19. Other employers will take a different tack, merely encouraging vaccines.” The report concludes:
“Especially given that EEOC has said COVID-19 poses a direct threat to the health and safety of [employees] and the general public, I imagine that the EEOC may be warmer to the idea of employer mandates than during the 2009 H1N1 pandemic when it suggested employers consider simply encouraging employees to be vaccinated. The EEOC’s final position and those of other government agencies remain to be seen, but regardless of whether mandates are merely tolerated or actively encouraged, employers will still have to consider legally required reasonable accommodations on a case-by-case basis.”