HealthLawBlog
Health care law (including regulatory and compliance issues, public health law, medical ethics, and life sciences), with digressions into constitutional law, statutory interpretation, poetry, and other things that matter
Tuesday, September 02, 2025
HealthLawBlog is moving to Substack
After 20+ years and over 1,100 posts here at Blogspot, I'm heading to Substack. You can get there by clicking this link. You can subscribe for free -- there's no charge and never will be. Thanks for supporting me here. I hope to see you over at Substack soon.
The CDC After Trump's & RFKJr's Friday Afternoon Massacre
- The signers are 9 former CDC directors (permanent or acting).
- They served during every Republican and Democrat administration from Jimmy Carter to Donald Trump.
- Their service as CDC directors goes back to 1977 -- collectively that represents over 100 years at the CDC.
- Despite their differences, they agree (as their title puts it) that "Kennedy Is Endangering Every American’s Health".
- What the health and human services secretary, Robert F. Kennedy Jr., has done to the C.D.C. and to our nation’s public health system over the past several months — culminating in his decision to fire Susan Monarez as C.D.C. director days ago — is unlike anything we had ever seen at the agency and unlike anything our country had ever experienced.
- Mr. Kennedy has fired thousands of federal health workers and severely weakened programs designed to protect Americans from cancer, heart attacks, strokes, lead poisoning, injury, violence and more.
- Amid the largest measles outbreak in the United States in a generation, he’s focused on unproven treatments while downplaying vaccines.
- He canceled investments in promising medical research that will leave us ill prepared for future health emergencies.
- He replaced experts on federal health advisory committees with unqualified individuals who share his dangerous and unscientific views.
- He announced the end of U.S. support for global vaccination programs that protect millions of children and keep Americans safe, citing flawed research and making inaccurate statements.
- And he championed federal legislation that will cause millions of people with health insurance through Medicaid to lose their coverage.
- Firing Dr. Monarez — which led to the resignations of top C.D.C. officials — adds considerable fuel to this raging fire.
- When Mr. Kennedy administered the oath of office to Dr. Monarez on July 31, he called her “a public health expert with unimpeachable scientific credentials.” But when she refused weeks later to rubber-stamp his dangerous and unfounded vaccine recommendations or heed his demand to fire senior C.D.C. staff members, he decided she was expendable.
- These are not typical requests from a health secretary to a C.D.C. director. Not even close. None of us would have agreed to the secretary’s demands, and we applaud Dr. Monarez for standing up for the agency and the health of our communities.
Wednesday, August 27, 2025
The CDC: Of Revolving Doors and Dark Clouds and Chopping Blocks, Oh My
Nothing has been said so far by either HHS or the White House that would shed light on the reason for her firing. Stories have been flying around about disquiet among CDC's rank and file employees following (1) the August 11 shooting at CDC headquarters in Atlanta that resulted in the death of a Dekalb County police officer, (2) mass layoffs at the CDC since January, (3) increased harassment of CDC employees by (among others) anti-vaxxers, and (4) chaos surrounding RFKJr's relentless dismantling of CDC's vaccine infrastructure, including the dismissal of all members of the agency's vaccine advisory panel and defunding mRNA vaccine research. (CBS News; NPR)
It hardly needs to be said that Dr. Monarez did not have a hand in any of these events and could hardly have turned the agency around against headwinds like these in less than a month on the job. Maybe Federal Housing Finance Agency Director Bill Pulte can unearth something wrong with her (pre-confirmation) home mortgage application, which seems to be the administration's preferred mode of political harassment these days (NBC, Aug. 27).
At this stage, it appears that the dark days at the CDC aren't going to lighten up anytime soon. And that's not good news for the rest of us.
Elections have consequences.
UPDATE (10:09pm CDT):
Late-breaking reports from the NY Times (and WaPo):
- Sources say the director was told by RFKJr to resign or be fired. The immediate issue was her refusal to support the unscientific policy against vaccines that had played out at HHS over the past 7 months.
- She was also told to fire key senior officials evidence-based policies toward vaccines differed from the Secretary's.
- Monarez refused to fire the senior officials and refused to resign.
- As of this evening:
- Monarez was fired as director of CDC. "[A]t 9:30 p.m. [EDT], a spokesman for President Trump, Kush Desai, said in an email message that Dr. Monarez had been terminated. . . . Susan Monarez is not aligned with the President’s agenda of Making America Healthy Again,” Mr. Desai wrote. . . . "Since Susan Monarez refused to resign despite informing HHS leadership of her intent to do so, the White House has terminated Monarez from her position with the C.D.C.”
- The following senior officials have resigned:
- Dr. Debra Houry, the C.D.C.’s chief medical officer;
- Dr. Demetre Daskalakis, who ran the center that issues vaccine recommendations;
- Dr. Daniel Jernigan, who oversaw the center that oversees vaccine safety; and
- Dr. Jennifer Layden, who led the office of public health data.
- Reactions to the firing and the resignations have been swift:
- Dr. Mandy Cohen, who ran the agency during the second half of the Biden administration, called the officials “exceptional leaders who have served over many decades and many administrations,” and warned that “the weakening of the C.D.C. leaves us less safe and more vulnerable as a country.”
- Dr. Anne Schuchat, the C.D.C.’s principal deputy director until her retirement in May 2021, called them “the best of the best.” “These individuals are physician-scientist public health superstars,” she said. “I think we should all be scared about the nation’s health security.”
Monday, August 25, 2025
Texas and Trump: Failing Grades on Abortion and Measles
1. Emergency obstetrical interventions delayed or withheld. Marin Wolf and her colleagues at the Dallas Morning News have published a series of articles ("Standard of Fear") beginning in the paper's Sunday (8/24) edition and continuing in the Monday (8/25) edition. (Warning: possible paywall.) An overview:
More than a year ago, The Dallas Morning News set out to explore how Texas’ overlapping abortion laws have altered the landscape of obstetric health care. Through more than 100 interviews with physicians and other health care professionals, researchers, advocates, legal experts, patients and family members, reporters documented deviations from the standard of care, as well as other unintended consequences.
A review of hundreds of pages of medical and death records, including the examination of more than a dozen patient cases, revealed how the laws have been sweeping in their collateral damage — with patients, families and medical providers caught in the middle.
Texas lawmakers have accomplished what they set out to do — criminalize and, thus, drastically reduce access to abortion. But in doing so, they have also derailed medical care for women trying to have children who developed heartbreaking or life-threatening problems in their pregnancies.
Many women — including those who never imagined they would want or need an abortion — have faced delays or denials of treatment. This includes patients with preexisting medical conditions that make pregnancy dangerous, ectopic pregnancies, miscarriages, the onset of labor before a fetus is viable and fetal diagnoses that are lethal or life-limiting. Others have grown too afraid of becoming pregnant in Texas — so much so that there has been an increase in surgical sterilizations.
In a state that leads the nation in maternal mortality, how can legislators possibly justify interfering with women's autonomy and making it more difficult to obtain potentially life-saving emergency obstetrical care?
2. CDC dropped the ball on the West Texas measles outbreak. KFF News published an article this morning ("As Measles Exploded, Officials in Texas Looked to CDC Scientists. Under Trump, No One Answered.") that documents the impact of Trump-era cuts in staffing and funding at the Centers for Disease Prevention and Control. Here are some excerpts:
As measles surged in Texas early this year, the Trump administration’s actions sowed fear and confusion among CDC scientists that kept them from performing the agency’s most critical function — emergency response — when it mattered most, an investigation from KFF Health News shows.
The outbreak soon became the worst the United States has endured in over three decades. . . .
Delays have catastrophic consequences when measles spreads in undervaccinated communities, like many in West Texas. If a person with measles is in the same room with 10 unvaccinated people, nine will be infected, researchers estimate. If those nine go about their lives in public spaces, numbers multiply exponentially.
The outbreak that unfolded in West Texas illustrates the danger the country faces under the Trump administration as vaccination rates drop, misinformation flourishes, public health budgets are cut, and science agencies are subject to political manipulation.
And here's the kicker:
While the Trump administration stifled CDC communications, health secretary Robert F. Kennedy Jr. fueled doubt in vaccines and exaggerated the ability of vitamins to ward off disease. Suffering followed: The Texas outbreak spread to New Mexico, Oklahoma, Kansas, Colorado, and Mexico’s Chihuahua state — at minimum. Together these linked outbreaks have sickened more than 4,500 people, killed at least 16, and levied exorbitant costs on hospitals, health departments, and those paying medical bills.
The federal-state public-health partnership was based upon indispensable monitoring data and expertise that could be mobilized in an instant to support local public-health officials working in affected communities to limit the damage of infectious disease. Instead, a bunch of no-nothings in this administration are ushering in a new Dark Age of illness and premature death.
Elections have consequences.
Friday, August 22, 2025
Providers with Larceny in Their Heart
- Three Baton Rouge Individuals Sentenced To Federal Prison In Connection With The Department Of Justice’s 2024 National Health Care Fraud Enforcement Action (August 21, 2025; U.S. Attorney's Office, Middle District of Louisiana)
- Brooklyn Cardiologist Sentenced To 37 Months In Prison In Connection With Health Care Fraud And Bribery Scheme (August 21, 2025; U.S. Attorney's Office, Southern District of New York)
- Memphis Woman Sentenced To Federal Prison For Scheme To Defraud Federal COVID-19 Relief Program (August 21, 2025; U.S. Attorney's Office, Western District of Tennessee)
- AG Murrill's Medicaid Fraud Control Unit Arrests Baton Rouge Woman For Failing To Report The Physical Abuse Of A Mentally Challenged Client As Required By Law (August 21, 2025; State of Louisiana)
- Saginaw Physician Charged With Medicaid Fraud (August 15, 2025; State of Michigan)
- Attorney General Griffin Announces Two Convictions And One Arrest By Medicaid Fraud Control Unit (August 15, 2025; State of Arkansas)
- 10 Medicaid Providers Facing Fraud, Theft Charges (August 15, 2025; State of Ohio)
- AG Murrill's Medicaid Fraud Control Unit Arrests Slidell Woman For Cruel Attack On An Individual With A Disability Under Her Care (August 15, 2025; State of Louisiana)
- Houma Woman Arrested By Louisiana Bureau Of Investigation For Falsifying Check Stubs And Underreporting Income To Defraud The Medicaid Program Of More Than $83,000 (August 15, 2025; State of Louisiana)
- Attorney General Raúl Torrez Files Lawsuit Alleging Over $1.6 Million In Fraudulent Medicaid Claims And Identity Theft Of Children (August 14, 2025; State of New Mexico)
- Attorney General Bonta Announces Arrest And Felony Charges Against Nursing Assistant For Alleged Sexual Assault Of Three Elderly Patients In Northern California (August 14, 2025; State of California)
Thursday, August 21, 2025
US DOJ Seeks Transgender Patient and Provider Information from Leading Pediatric Hospital
The KFF articles reports that DOJ also seeks "billing documents, communication with drug manufacturers and data such as . . . emails, Zoom recordings, 'every writing or record of whatever type' doctors have made, voicemails and text messages on encrypted platforms dating to January 2020 — before hormone therapy, puberty blockers and gender transition surgery had been banned anywhere in the United States."
As reported by the Washington Post (Aug. 20):
Jacob T. Elberg, a former federal prosecutor specializing in health care fraud, said Bondi’s statement suggests the government “is using its investigative powers to target medical providers based on a disagreement about medical treatment rather than violations of the law.”
When she announced the subpoenas last month, AG Pam Bondi said DOJ was seeking to hold “medical professionals and organizations that mutilated children in the service of a warped ideology” accountable. Considering the broad professional support for supportive treatments, you have to ask whose "warped ideology" is behind the subpoenas.
The Bloomberg Law story provides a good collection of articles on the Trump administration's escalating war on transgender medicine:
- Trump Signals Gender Overhaul While Health Policy Changes Wait; Jan. 21, 2025,
- Some Hospitals Pausing Youth Transgender Care Are Skirting Law; Feb. 20, 2025
- HHS Doubts Benefit of Gender-Affirming Care for Children (2); May 1, 2025
- Trump FTC Chair Looks for Deception in Gender-Affirming Care (2); July 9, 2025
- Trump Actions on Gender Care for Minors Draw New States Lawsuit (1); Aug. 1, 2025
Thursday, August 07, 2025
Trump Administration Plans to Burn $9.7 Million in Contraceptive Medicines and Devices
Diverting these reproductive health supplies will have a devastating effect:
Siobhan Perkins, who was the procurement adviser for the U.S.A.I.D. contraception supply chain, said the products slated for destruction were enough to prevent approximately 362,000 unintended pregnancies, 110,000 unsafe abortions and 718 maternal deaths.
Destruction of the contraceptives will cost $160,000 in transportation and incineration charges, but -- as reported by Reuters -- there's a low-cost option that, with any other administration, would be a win-win solution:
Sarah Shaw, Associate Director of Advocacy at MSI Reproductive Choices, told Reuters the non-profit organisation had volunteered to pay for the supplies to be repackaged without USAID branding and shipped to countries in need, but the offer was declined by the U.S. government.
"MSI offered to pay for repackaging, shipping and import duties but they were not open to that... We were told that the U.S. government would only sell the supplies at the full market value," said Shaw.
She did not elaborate on how much the NGO was prepared to pay, but said she felt the rejection was based on the Trump's administration's more restrictive stance on abortion and family planning.
"This is clearly not about saving money. It feels more like an ideological assault on reproductive rights, and one that is already harming women."
This decision is part of a war on women's health that is, in economic terms, stupid and, in moral terms, evil. How much lower can this crowd go?
Tuesday, July 29, 2025
Maternal Mortality: Elections Have Consequences
The United States has long had the worst maternal mortality rate of any wealthy nation — a rate that soared during the COVID-19 pandemic, peaking in 2021.
A new Commonwealth Fund report analyzes the latest national data on maternal mortality and offers a broad look at the causes and characteristics of preventable maternal deaths, including sharp differences linked to race and geography.
Among the key findings:
- Pregnancy-related mortality is 18 to 49 percent higher in states that haven’t expanded Medicaid eligibility, compared to those that have.
- Maternal death rates in rural areas are more than 50 percent higher than in large urban areas.
- The pandemic deepened racial disparities, with Black, Hispanic, and American Indian/Native women facing the highest risks.
While maternal mortality has nearly returned to pre-pandemic levels, the outlook remains troubling. Looming federal budget cuts could reverse recent gains and significantly increase preventable maternal and infant deaths. [Emphasis added]
The data in the report are truly eye-popping. Here's an example I wasn't expecting: A significant majority of maternal deaths occur in the year following birth -- i.e., after the obstetrician and various other health professionals have done their work.
Saturday, July 26, 2025
U.S. Preventive Services Task Force: Now You See It, Soon You Won't
Fortunately, that didn't happen. The USPSTF is responsible for creating the lists of services that health insurers must cover without collecting copays or deductibles from their insureds under the Affordable Care Act. In effect, then, this litigation was yet another attempt to eviscerate a basic part of Obamacare. And the Court, yet again, resisted the invitation to do so.
The victory, however, may be short-lived. The majority opinion by Justice Kavanaugh made it very clear that, because the task force's members were "inferior officers," the Secretary of HHS -- and not the President -- could not only appoint members but also remove them:
[B]ecause the Secretary of HHS appoints the Task Force members, he also has the authority to remove the Task Force members at will. . . . When a statute empowers a department head to appoint an officer, the default presumption is that the officer holds his position “at the will and discretion of the head of the department,” even if “no power to remove is expressly given". . . . The Secretary of HHS has the power to appoint (and has appointed) the Task Force members. And no statute restricts removal of Task Force members. Therefore, “there can be no doubt” that the Secretary may remove Task Force members at will.
This was an important part of the Court's conclusion that members of the task force are "inferior officers" and were, therefore, properly appointed by the Secretary.
This "win," however, leads directly to headlines in the past few days that RFK, Jr. is ready to fire all of the current members of the task force, apparently because they are too "woke." (Reuters, WSJ, NBC, Daily Beast). Can he really do that? Of course he can; the Court said so in June. And it would be an exercise of the same removal power that led to his removal of all 17 members of the Advisory Committee on Immunization Practice on June 8, replacing them with, among others, vaccine skeptics.
The "wokeness" of the USPSTF was the subject of an opinion piece in The American Conservative. The author singles out three initiatives of the USPSTF: (1) increasing awareness of systemic racism in clinical medicine, (2) being attentive to issues of sex and gender in clinical settings, and (3) including "preventive prophylaxis for HIV, commonly known as PrEP, for individuals at risk of infection with that disease. As the author explains:
This population consists almost entirely of sexually active gay men, which has led a number of Christian employers who provide insurance to protest that the ACA (and its instrument, the USPSTF) are requiring them to subsidize activities they oppose on moral and religious grounds.
The author describes these initiatives as "sinister . . . abuses" that should be eliminated from medical practice. Some of the reporting on RFK, Jr.'s plan indicate that he is bothered by the task force's "wokeness" and cite this article as one source of his concerns.
Different health outcomes for racial minorities, women, gay persons, and transgendered individuals are well-established. Firing task force members won't make the issues go away. But President Trump knew exactly what he was doing when he put his man in charge of HHS.
An excellent piece by Yale Law School's Abbe Gluck teases out further implications of the Supreme Court's opinion: "Braidwood is an opinion that, to the relief of many, saves the ACA once again. But it leaves open critical questions about the future of respect for scientific expertise and how those questions will inevitably be litigated."
Thursday, July 24, 2025
Organ Donation After Cardiac Death
DCD protocols were developed as a way of obtaining transplantable organs without waiting for brain death to occur. Considering the 103,000+ backlog of transplant candidates on national waiting lists, DCD seemed like an innovative way to increase the supply of organs.
The protocol called for taking away life-support, waiting for spontaneous respirations and cardiac function to stop, waiting a little longer to ensure that the donor's heart didn't spontaneously restart ("autoresuscitation), and declaring death. All of these steps take place in an operating room where a transplant team is ready to remove the decedent's organs while they are still relatively "fresh."
Criticisms were mostly focused on the waiting periods, which -- if too short -- might result in taking vital organs from a patient who wasn't really dead. With the encouragement of the transplant field's regulatory body -- the United Network for Organ Sharing (UNOS) -- the practice has established a solid footing and currently accounts for 43% of deceased donors, 7,200 donors in total.
If there's a problem with DCD, it is the persistent reports of DCD donors being declared dead and turning out not to be. As recently as this week, The New York Times ran a long story with the striking headline, "Doctors Were Preparing to Remove Their Organs. Then They Woke Up". Experts say that if the protocol is carried out properly, this should never happen. So what's the explanation? The agency that oversees the federal Organ Procurement and Transplant Network is the Health Resources and Services Administration (HRSA), which conducted a review of cases in Kentucky. As reported by the Times:
Now, a federal investigation has found that officials at the nonprofit in charge of coordinating organ donations in Kentucky ignored signs of growing alertness not only in that patient but also in dozens of other potential donors.
The investigation examined about 350 cases in Kentucky over the past four years in which plans to remove organs were ultimately canceled. It found that in 73 instances, officials should have considered stopping sooner because the patients had high or improving levels of consciousness.
The results of that investigation has led HHS to start a process of "reforming" the OPTN:
[HHS] announced a major initiative to begin reforming the organ transplant system following an investigation by its Health Resources and Services Administration (HRSA) that revealed disturbing practices by a major organ procurement organization.“Our findings show that hospitals allowed the organ procurement process to begin when patients showed signs of life, and this is horrifying,” Secretary Kennedy said. “The organ procurement organizations that coordinate access to transplants will be held accountable. The entire system must be fixed to ensure that every potential donor’s life is treated with the sanctity it deserves.”
The headline of this press release is apparently intended to alarm: HHS Finds Systemic Disregard for Sanctity of Life in Organ Transplant System (boldface in original). The question this leaves open is whether HHS is going to adopt measures to ensure compliance with the existing DCD protocol or take steps to scrap DCD altogether. (Wait until RFK, Jr. is told about Nomothermic Regional Perfusion!) Stay tuned . . . .
Monday, July 14, 2025
The Administration's Three-Pronged Assault on Health Care
The three fronts of this assault—on tax-funded medical coverage, public health, and medical research—have overlapping aims. The campaign to slash Medicaid—relied on by the poor since its establishment in 1965—follows a long neoliberal tradition of prescribing austerity for the working class and largesse for the rich. Trump and his allies seem to view public health, for its part, as waste that can be excised (DOGE-style) to fund tax cuts, as a source of regulatory excess that constrains profit-making, and as a locus of “woke” ideology and inconvenient facts. The assault on medical research is driven by similar concerns, with the added benefit of dominating rival centers of power like universities and the professions.
The cuts to Medicaid and Medicare are incredibly short-sighted and cruel. The cuts to medical research are bound to lead to increases in morbidity and mortality. And the cuts to public health initiatives is particularly foolish. The authors write:
This funding squeeze is without historical parallel. Yet it also bears stressing that public health agencies have long been underfunded and neglected. Unlike medical care—which almost everyone periodically encounters when they go to a doctor or an emergency room—the equally essential work of public health is often invisible. Americans’ life expectancy soared by more than twenty years in the first half of the twentieth century, mainly owing to public health measures like safe drinking water, rather than to improvements in medical care. In more recent decades public health measures, like those that decreased air pollution and smoking, have been responsible for about half of life expectancy gains.
For all that, public health initiatives have been historically underfunded. As a component of overall health expenditures, it's accounted for 3 percent in 2024:
Gutting public-health infrastructure and programs puts barely a dent in the projected deficits of the One Big Beautiful Act bill,** so something else is going on here.
Trump and his MAGA supporters fervently believe that the federal (and some state) public health authorities -- CDC: They are talking about you -- overplayed their hands during COVID: too many mandates (vaccines, masks) and not enough individual choice. This ignores at least two points: (1) public health is the antithesis of autonomy and self-determination,; it prioritizes community health over individual choice -- always has and always will, and (2) the mandates probably saved hundreds of thousands if not millions of lives. Were they onerous? Burdensome? Possibly broader than they needed to be? Yes, yes, and maybe. But taking funds away from research and public health initiatives, not to mention Medicare and Medicaid, is a gross overreaction to the 2020-24 response to COVID. And down the road we will all pay the price for this woefully benighted policy.
___________________
* Contact me offline for a PDF of the article, which I share solely for the purpose encouraging you to subscribe to this outstanding publication.
** No longer the official name of the law signed by the president on July 4 (here).
Sunday, July 13, 2025
Just When You Thought It Couldn't Get Crazier . . . .
News sources report that yesterday our dear leader has decided it may be time to revoke Rosie O'Donnell's citizenship. He posted on Truth Social: “Because of the fact that Rosie O’Donnell is not in the best interests of our Great Country, I am giving serious consideration to taking away her Citizenship,” Trump wrote in a social media post on Saturday. He added that O’Donnell, who moved to Ireland in January, should stay in Ireland “if they want her.” (AP, CNN, Fox News, NY Times)
There are a few possible explanations for what is going on here:
- Argle-bargle: Trump can't possibly believe he or anyone else in the federal government can strip Rosie O'Donnell of her citizenship, which -- according to the XIVth Amendment -- was and is her birthright. Trump's intemperate threats to violate the Constitution come as easily to him as pounding sand and are just about as meaningful. These are the outbursts of a man-child mid-tantrum.
- Media hog: Nobody in public life is quite as good as Trump at capturing and keeping the spotlight on himself. This is how it's done, ladies and gentlemen. For aspiring oligarchs, watch and learn.
- Keep the base riled up: Most voters in this country don't know much about the Privileges and/or Immunities Clauses of Article IV and Amendment XIV of the Constitution or the Naturalization Act of 1906. Wild statements about denaturalizing a person who is a citizen by birth may appeal to some Trump supporters for whom a social media rant is a nearly free piece of red meat.
- He hates her. He really hates her: The President dismisses those who either disagree with him or even accurately report on his mis- and disinformation as suffering from "Trump Derangement Syndrome". After years of picking fights with Rosie O'Donnell, Trump is exhibiting signs of O'Donnell Derangement Syndrome. There seem to be few people who can set Trump off the way Rosie does, and when that happens, the poor fellow can't think straight.
- Remember, Trump is a fan of professional wrestling. The match is scripted in advance, the violence is mostly fake, and the storylines are hatched by executives who are experts at hyping the crowd. The wrestlers know it's fake, and so does the audience, but the wrestlers are making good money and the audience loves the entertainment. It doesn't matter that it's only a show. So are the movies and TV shows, but we still care even if the blood and gore are fake. Give the people bread and circuses is never a bad strategy.
- He believes his own nonsense. It doesn't seem likely, but he may truly believe that the presidency comes with kingly powers and royal prerogatives that are unbounded by statutes and the Constitution. His record since January 20 certainly suggests that "the rule of law" means nothing to him, and neither Congress nor the Supreme Court seem particularly interested in reeling in his autocratic aspirations.
Saturday, July 12, 2025
The Outrageous Upside-Down World of the Department of Justice
According to court documents, Dr. Michael Kirk Moore Jr., 58, of Salt Lake County, Utah and his co-defendants, listed below including his neighbor, ran a scheme out of Plastic Surgery Institute of Utah Inc. to defraud the United States and the Centers for Disease Control and Prevention (CDC). The defendants allegedly destroyed at least $28,028.50 worth of government-provided COVID-19 vaccines, and distributed at least 1,937 doses’ worth of fraudulently completed vaccination record cards to others in exchange for either direct cash payments or required “donations” to a specified charitable organization, without administering a COVID-19 vaccine to the card recipient. As charged in court documents, defendants also administered saline shots to minors – at the request of their parents – so children would think they were receiving a COVID-19 vaccine.
At the time, this was considered fairly reprehensible behavior:
"By allegedly falsifying vaccine cards and administering saline shots to children instead of COVID-19 vaccines, not only did this provider endanger the health and well-being of a vulnerable population, but also undermined public trust and the integrity of federal health care programs,” said Curt L. Muller, Special Agent in Charge with the Department of Health and Human Services, Office of the Inspector General. . . . “This defendant allegedly used his medical profession to administer bogus vaccines to unsuspecting people, to include children falsifying a sense of security,” said Acting Special Agent in Charge Chris Miller, HSI Las Vegas.
That was then; this is now.
True to form, this morning Attorney General Pam Bondi announced on X that she has directed the U.S. Attorney to move to dismiss the charges against Dr. Moore. As reported by CBS News:
"Dr. Moore gave his patients a choice when the federal government refused to do so. He did not deserve the years in prison he was facing. It ends today," Bondi wrote on X, thanking Rep. Marjorie Taylor Greene, who has a history of casting doubts on the efficacy of COVID vaccines, for raising awareness of his case. "She has been a warrior for Dr. Moore and for ending the weaponization of government," Bondi wrote.
In a post on X on Saturday, Greene called Moore a "hero who refused to inject his patients with a government mandated unsafe vaccine!"
HHS Secretary RFK, Jr. is on-board with this:
Health Secretary Robert F. Kennedy Jr., who for decades has sown doubt about the safety of vaccines contrary to evidence and research by scientists, wrote on X in April: "Dr. Moore deserves a medal for his courage and his commitment to healing!" (Jerusalem Post, July 12).
Hero? Neither AG Bondi nor Rep. MJT suggests the factual allegations that support the federal grand jury's indictment are not true. On that basis, Dr. Moore is a Public Health Enemy. But not to an administration that considered 1,575 insurrectionists hell-bent on subverting the 2020 presidential election "heroes."
Friday, July 11, 2025
New England Journal of Medicine: How the Supreme Court Got the Tennessee Transgender Case Wrong
"[s]urgically removing, modifying, altering, or entering into tissues, cavities, or organs of a human being,” or “[p]rescribing, administering, or dispensing any puberty blocker or hormone,” for the purpose of (1) “[e]nabling a minor to identify with, or live as, a purported identity inconsistent with the minor’s sex,” or (2) “[t]reating purported discomfort or distress from a discordance between the minor’s sex and asserted identity” (citations omitted).
The author starts -- as did Chief Justice Roberts in his opinion for the majority -- with a brief recitation of the misery and suffering the Tennessee ban virtually guarantees. That, of course, is not enough of a reason to strike down a state statute, even one as cruel and misguided as Tennessee's -- not to mention the similar laws in 20 additional states.
The fate of the plaintiffs' challenge to the Tennessee statute turns, as is so often the case, on the lawyerly notion of standard of review. The phrase refers to the lens through which challenged statutes are viewed and required different levels of justification from the government when its law is challenged on Equal Protection of Due Process grounds (among others). At one end of the spectrum is "rational basis" review. The question for a reviewing court is two-fold: (1) is there any conceivable governmental interest -- whether it was considered by the enacting legislature or not -- that is furthered by the law, and (2) is the law reasonably related to that interest. Sound like a slam-dunk for the state? It almost always is. The last time I looked, only five laws have ever flunked the rational-basis test (though, like nearly everything else in Constitutional Law, that number is debated). Most laws get this extremely low level of judicial review, so when the Court chooses that standard of review, it's usually lights out for the challenger.
There are, however, a couple of higher standards of review -- "intermediate scrutiny" and "strict scrutiny." Strict scrutiny is exceedingly difficult for the government to satisfy; the late Stanford law prof Gerald Gunther described it as "strict in theory, fatal in fact." (That was surely an overstatement; historically governments have enjoyed a non-zero success rate in such cases of 30%.)
Discrimination on the basis of sex, however, requires the government to justify its law under the more forgiving review standard of "intermediate scrutiny" (sometimes referred to as "heightened scrutiny" or "rational basis with teeth"). To succeed under this standard, the government must prove that it is pursuing an important governmental interest and that the law in question is substantially related to that important governmental interest.
So the controlling question in Skrmetti came down to this: Was the Tennessee legislature's ban on most treatments for transgender minors a distinction based upon sex. If yes, intermediate scrutiny would be triggered, making it materially more difficult for the state to get a favorable ruling The Sixth Circuit Court of Appeals said the ban did not implicate sex and upheld the statute under rational basis review. The Supreme Court agreed with the Sixth Circuit and affirmed.
The result at first (and second and third) blush is surprising. As the quotes from the law at the top of this post show, the law is riddled with references to "sex." The majority justices tied themselves into knots in their effort to avoid that characterization, concluding (in the words of Chief Justice Roberts) that the law "prohibits healthcare providers from administering puberty blockers or hormones to minors for certain medical uses, regardless of a minor’s sex." If the law doesn't discriminate on the basis of sex, rational basis review applies and, as usual, the law easily passes the lowest level of review.
Prof. Skinner-Thompson argues that this conclusion is based on two logical errors. First, he relies on an argument made by Justice Sotomayor in dissent:
[A]s Justice Sonia Sotomayor points out in her dissent, the excluded medical purpose is defined with reference to a person’s sex: “Key to whether a minor may receive puberty blockers or hormones is whether the treatment facilitates the ‘medical purpose’ of helping the minor live or appear ‘inconsistent with’ the minor’s sex. That is why changing a patient’s sex yields different outcomes” under the statute.
Skinner-Thompson's second argument concerns transgender discrimination:
The majority concludes that the statute does not exclude people on the basis of transgender status but instead “removes one set of diagnoses — gender dysphoria, gender identity disorder, and gender incongruence — from the range of treatable conditions.”
This interpretation is plainly wrong; the statute specifically excludes minors who “identify with” a gender inconsistent with their sex assigned at birth from receiving the relevant treatments. Even Justice Samuel Alito in his concurrence notes that “a strong argument” exists that the statute imposes a classification on the basis of transgender identity. But he, like Justices Amy Coney Barrett and Clarence Thomas, would conclude that drawing lines on the basis of transgender identity does not trigger heightened scrutiny — a question that the majority opinion avoids.
The Court's opinion in Skrmetti offers a green light to all state legislators who are itching to deny appropriate medical treatment for transgender youth. The majority does what it can to conjure up medical doubt about these medical treatments, but the Tennessee law was opposed by a dizzying array of relevant medical associations. See Brief of Amici at p. 13 et seq. Their brief begins:
The [Tennessee law] prohibits healthcare providers from providing patients under the age of 18 with critical, medically necessary, evidence-based care for gender dysphoria. Denying such evidence-based medical care to adolescents who meet the requisite medical criteria puts them at risk of significant harm. Below, amici provide the Court with an accurate description of the relevant treatment guidelines and summarize the scientific evidence supporting the genderaffirming medical care for adolescents that is prohibited by [Tennessee]. (footnotes omitted; emphasis added)
To which six justices of the Supreme Court said "Meh."
Wednesday, July 09, 2025
U.S. Measles Cases Reach 33-Year High
“The most effective way to prevent the spread of measles is the M.M.R. vaccine,” he added, referring to the measles, mumps and rubella vaccine.At the same time, Mr. Kennedy has stopped short of recommending universal vaccination in communities where the virus is not spreading.And he has ordered a re-examination of whether the vaccine causes autism, a claim long ago debunked by research, to be conducted by a well-known vaccine skeptic.
And as of this morning:
In a statement to NPR, Health and Human Services Department spokesperson Andrew Nixon said, "CDC continues to recommend MMR vaccines as the best way to protect against measles. The decision to vaccinate is a personal one." [emphasis added]
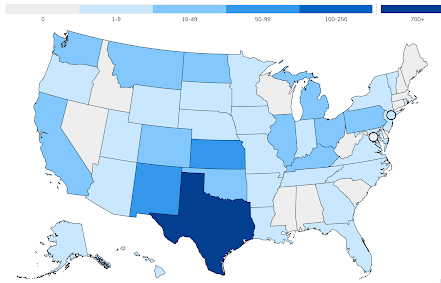
According to the World Health Organization, "herd immunity" for measles requires at least a 95% immunization rate, which is a standard only 11 states currently achieve.
The lower the rate falls below 95%, the greater the risk to the community of an outbreak. Of the 40 remaining jurisdictions, 12 states have a vaccination rate below 90%.
One of the contributing factors to the low rate of vaccination is permissive state laws that allow parents to opt their kids out of compulsory-vaccination for public-school enrollment. All states require some vaccinations, including the MMR (measles, mumps, and rubella) vaccine. But only 5 states limit parental exemptions to medical reasons. All 46 remaining jurisdictions add non-medical reasons for exemptions, including: religious, personal belief, or both.
Source: National Conference of State Legislatures
As expected, there is an almost-perfect correlation between these two maps: the vaccination rates >94% tend to be in the states that limit their vaccination exemptions to individual medical indications.
The justification for non-medical exemptions is primarily -- if not entirely -- political, not legal. Although the issue has divided lower courts, one COVID-era Supreme Court opinion provides support for states that exclude religious reasons for vaccine exemptions as long as the state requirement is applied equally to religious and secular settings. Indeed, cases going back to the military draft during the Vietnam War -- cases that struggled to define and apply the draft law's religious exemption -- observed that Congress was not required to include a religious exemption at all (but when it does, it must do so without favoring one set of religious beliefs over others).
Tuesday, July 08, 2025
Larry Summers: One Big Beautiful Bill Act* is Shameful
A few highlights:
- "[A] focus on macroeconomics, while valid, misses the human brutality that I now see as the most problematic aspect of the legislation. I don’t remember on any past Fourth of July being so ashamed of an action my country had just taken." By the way, the headline for this op-ed -- presumably provided by a line editor at the paper -- erroneously stated "This Law Made Me Ashamed of My Country." Big difference.
- "This round of budget cuts in Medicaid far exceeds any other cut the United States has made in its social safety net. The approximately $1 trillion reduction, over 10 years, represents about 0.3 percent of gross domestic product. Previously, the most draconian cuts came with President Ronald Reagan’s 1981 tax law. But they were far smaller — $12 billion over 10 years and 0.03 percent of G.D.P. The Trump law will remove more than 11 million people from the rolls, compared with about three million under the Reagan cuts. Other noteworthy reductions to the social safety net, such as the Clinton-era welfare reform, were even smaller."
- "A number of studies suggest that removing one million people from the rolls for one year could result in about 1,000 additional deaths. It follows that removing more than 11 million people for a decade would probably result in more than 100,000 deaths. Because this figure fails to take account of the degradation of service to those who remain eligible — fewer rides to the hospital, less social support — it could well be an underestimate."
- "The cruelty of these cuts is matched only by their stupidity. Medicaid beneficiaries will lose, but so will the rest of us. The cost of care that is no longer reimbursed by Medicaid will instead be borne by hospitals and passed onto paying patients, only at higher levels, because delayed treatment is more expensive. When rural hospitals close, everyone nearby loses. Hospitals like the one where my daughters practice can no longer accept emergencies by air because those beds are occupied by patients with chronic diseases and no place to go."
- "Because of the congressional instinct for political survival, the Medicaid cuts are backloaded beyond the 2026 midterms. Cynicism may have a silver lining. As more people realize what is coming, there is time to alter these policies before grave damage is done. TACO — Trump always chickens out — is a doctrine that should apply well beyond financial markets."
________________
* No longer the obnoxiously titled "One Big Beautiful Act" Bill, it's now simply "An Act to provide for reconciliation pursuant to title II of H. Con. Res. 14." There's a story behind the name change, courtesy of something called the Byrd Rule. The authoritative congress.gov version is at the top of this post. The "official" reference is Pub. L. No. 119-21.
** Summers: "Last week, Robert Rubin and I warned of the many macroeconomic risks created by the domestic policy bill President Trump signed into law on Friday. I stand by our judgment that it will most likely slow growth, risk a financial crisis, exacerbate trade deficits and undermine national security by exhausting the government’s borrowing capacity. This is more than ample reason to regret its passage."
Tuesday, July 01, 2025
DOJ's Annual Health Care Fraud Takedown Nets Record Charges
The Justice Department today announced the results of its 2025 National Health Care Fraud Takedown, which resulted in criminal charges against 324 defendants, including 96 doctors, nurse practitioners, pharmacists, and other licensed medical professionals, in 50 federal districts and 12 State Attorneys General’s Offices across the United States, for their alleged participation in various health care fraud schemes involving over $14.6 billion in intended loss. . . .
I would guess that most if not all of the investigations that resulted in these charges began under President Biden. We can be thankful that the enforcement program wasn't reflexively derailed by the new leaders of DOJ.
Click here for more details of the largest Takedown (in dollars) in history.
Monday, June 30, 2025
Tracking the Changes in the Senate's Reconciliation Bill (Updated Daily)
Sunday, June 29, 2025
The Coming Health Care Apocalypse
After a quick review of what Obamacare did and didn't accomplish, Krugman writes:
[I]t led to a large decline in the number of Americans without health insurance. It also led to a large reduction in anxiety among Americans with preexisting conditions, who no longer had to fear being denied coverage or being trapped in jobs with health benefits for fear of losing coverage.
Essentially all these gains are about to be wiped out.
Apocalyptic sounds about right. Here's a graphic representation of the impact:
Basically, we’re talking about undoing all the progress America has made in expanding health insurance. And as I said, many independent analysts believe it could be substantially worse.Remember, this isn’t happening to save money: If Republicans cared about the deficit, they could forego those tax cuts. It isn’t happening by popular demand: the Big Beautiful Bill is extremely unpopular already, and will become even more unpopular once people see its effects.
So why is this happening? Krugman's take on the situation is hard to resist:
It’s happening because our government has been taken over by fanatics who believe that, one way or another, they can escape the electoral consequences of making millions of Americans’ lives much, much worse.
___________________________
* You can follow Krugman for free on Substack or, for a small monthly fee, you can get extended commentary. Either way, it's a good deal.
Friday, June 27, 2025
Trump Administration v. Rule of Law Redux
Professor Austin Sarat (Amherst College) is all over this one, arguing that the DOJ effort in this case shows yet again the disdain this administration has for the rule of law. It's a brief op-ed in Slate and worth the four minutes it takes to read.
As I wrote on Wednesday, respect for the rule of law -- particularly the law of the Constitution -- is exactly what our officials swear to uphold when they take their oath of office. And the Trump lawyers, among and above all others, should know better.
None of this bodes well for future health-law cases, which depend upon a fair reading of constitutional and statutory precedents, not the current DOJ's strong suit.
Thursday, June 26, 2025
The Supreme Court's "Disastrous Decision"
- Sotomayor, J.:
In matters of life and death, it is best to proceed with caution. In this case, the Government took the opposite approach. It wrongfully deported one plaintiff to Guatemala, even though an Immigration Judge found he was likely to face torture there. Then, in clear violation of a court order,
it deported six more to South Sudan, a nation the State Department considers too unsafe for all but its most critical personnel. An attentive District Court’s timely intervention only narrowly prevented a third set of unlawful removals to Libya.
Rather than allowing our lower court colleagues to manage this high-stakes litigation with the care and attention it plainly requires, this Court now intervenes to grant the Government emergency relief from an order it has repeatedly defied. I cannot join so gross an abuse of the Court’s equitable discretion. . . .
It is axiomatic, moreover, that when Congress enacts a statutory entitlement, basic procedural due process protections attach. Mathews v. Eldridge, 424 U. S. 319, 332 (1976). Congress expressly provided noncitizens with the right not to be removed to a country where they are likely to be tortured or killed. See 8 U. S. C. §1231 note. As this Court has explained, the “‘right to be heard before being condemned to suffer grievous loss of any kind . . . is a principle basic to our society.’” Mathews, 424 U. S., at 333 (quoting Joint Anti-Fascist Refugee Comm. v. McGrath, 341 U. S. 123, 168 (1951) (Frankfurter, J., concurring)). Being deprived of the right not to be deported to a country likely to torture or kill you plainly counts. Thus, plaintiffs have a right to be heard. . . .
There is no evidence in this case that the Government ever did determine that the countries it designated (Libya, El Salvador, and South Sudan) “w[ould] not torture” the plaintiffs. Application for Stay of Injunction 29. Plaintiffs merely seek access to notice and process, so that, in the event the Executive makes a determination in their case, they learn about it in time to seek an immigration judge’s review. The Fifth Amendment unambiguously guarantees that right. . . .
The Due Process Clause represents “the principle that ours is a government of laws, not of men, and that we submit ourselves to rulers only if under rules.” Youngstown Sheet & Tube Co. v. Sawyer, 343 U. S. 579, 646 (1952) (Jackson, J., concurring). By rewarding lawlessness, the Court once again undermines that foundational principle. Apparently, the Court finds the idea that thousands will suffer violence in farflung locales more palatable than the remote possibility that a District Court exceeded its remedial powers when it ordered the Government to provide notice and process to which the plaintiffs are constitutionally and statutorily entitled. That use of discretion is as incomprehensible as it is inexcusable. Respectfully, but regretfully, I dissent.
- Vladeck:
As long-time readers of this newsletter know, I’m not prone to hyperbole. But the title of this piece refers to today’s ruling as “disastrous.” In my view, that’s true for two reasons:
First, it is going to have massive effects. Keep in mind that, in a pair of similarly unexplained grants of emergency relief to the Trump administration last month, the Court cleared the way for the government to treat as many as one million migrants as removable who weren’t previously (including those with “temporary protected status” and those covered by a humanitarian parole program started by the Biden administration. Those folks can now not only be placed in removal proceedings, but even if they can’t be removed to their countries of origin, they can apparently be removed to other countries without additional process—at least until and unless something changes.
Second, and even more importantly, here is one of the most stark examples to date of the Trump administration overtly defying rulings by a federal district judge. Indeed, it did so twice in this case. For the Court to not only grant emergency relief in this case, but to offer nary a word of explanation either in criticism of the government’s behavior, or in defense of why it granted relief notwithstanding that behavior, is to invite—if not affirmatively enable—comparable defiance of future district court orders by the government. I would’ve thought that this was a message that this Supreme Court would be ill-inclined to send, even (if not especially) implicitly. But it’s impossible to imagine that the Trump administration will view it any other way. - Stohr:
[T]he Supreme Court’s majority has essentially washed its hands of its role in upholding the rule of law, the foundational principle that laws are meant to be followed by everyone, the government included, if we are to have a just society.
I don’t know how this court comes back from such an astonishing abrogation of its role at the top of a separate, coequal branch of government tasked with, among other things, being a check against tyranny from the executive branch. If last year’s ruling granting Trump broad immunity for illegal acts committed during his presidency was the shot, this week’s order was the bitter chaser.
For all the litigants (present and future) whose legal arguments depend upon the Court's interpretation of the Due Process and Equal Protection Clauses of the Constitution, hold onto your seats. If this case is any indication, it's going to be a bumpy ride.