 Today's New York Times has an article on the virtually unimpeachable argument in favor of a single-payer health-care financing system for the United States. All the arguments are there (except for one, which may be implicit in the others: we could provide universal coverage and still save a bundle). The article also recognizes that the great stumbling block isn't economics or logic: it's political. The American public simply doesn't believe the arguments and certainly doesn't trust the government to get it right. And although we already have a single-payer system for the elderly and disabled (Medicare), the military and their dependents (VA and CHAMPUS), and the most indigent of the indigent (Medicaid), which includes a substantial percentage of the children in this country, we still don't trust the government to get it right. If the author of this article is correct ("What is the most pressing problem facing the economy? A good case can be made for the developing health care crisis. Soaring costs, growing ranks of uninsured and a steady erosion of corporate health benefits add up to a giant drag on the nation’s future prosperity."), this ought to be domestic policy issue #1 between now and the 2008 elections. But I'm not taking any bets.
Today's New York Times has an article on the virtually unimpeachable argument in favor of a single-payer health-care financing system for the United States. All the arguments are there (except for one, which may be implicit in the others: we could provide universal coverage and still save a bundle). The article also recognizes that the great stumbling block isn't economics or logic: it's political. The American public simply doesn't believe the arguments and certainly doesn't trust the government to get it right. And although we already have a single-payer system for the elderly and disabled (Medicare), the military and their dependents (VA and CHAMPUS), and the most indigent of the indigent (Medicaid), which includes a substantial percentage of the children in this country, we still don't trust the government to get it right. If the author of this article is correct ("What is the most pressing problem facing the economy? A good case can be made for the developing health care crisis. Soaring costs, growing ranks of uninsured and a steady erosion of corporate health benefits add up to a giant drag on the nation’s future prosperity."), this ought to be domestic policy issue #1 between now and the 2008 elections. But I'm not taking any bets.
Health care law (including regulatory and compliance issues, public health law, medical ethics, and life sciences), with digressions into constitutional law, statutory interpretation, poetry, and other things that matter
Sunday, December 31, 2006
Single-payer system for the US: you heard it here last
 Today's New York Times has an article on the virtually unimpeachable argument in favor of a single-payer health-care financing system for the United States. All the arguments are there (except for one, which may be implicit in the others: we could provide universal coverage and still save a bundle). The article also recognizes that the great stumbling block isn't economics or logic: it's political. The American public simply doesn't believe the arguments and certainly doesn't trust the government to get it right. And although we already have a single-payer system for the elderly and disabled (Medicare), the military and their dependents (VA and CHAMPUS), and the most indigent of the indigent (Medicaid), which includes a substantial percentage of the children in this country, we still don't trust the government to get it right. If the author of this article is correct ("What is the most pressing problem facing the economy? A good case can be made for the developing health care crisis. Soaring costs, growing ranks of uninsured and a steady erosion of corporate health benefits add up to a giant drag on the nation’s future prosperity."), this ought to be domestic policy issue #1 between now and the 2008 elections. But I'm not taking any bets.
Today's New York Times has an article on the virtually unimpeachable argument in favor of a single-payer health-care financing system for the United States. All the arguments are there (except for one, which may be implicit in the others: we could provide universal coverage and still save a bundle). The article also recognizes that the great stumbling block isn't economics or logic: it's political. The American public simply doesn't believe the arguments and certainly doesn't trust the government to get it right. And although we already have a single-payer system for the elderly and disabled (Medicare), the military and their dependents (VA and CHAMPUS), and the most indigent of the indigent (Medicaid), which includes a substantial percentage of the children in this country, we still don't trust the government to get it right. If the author of this article is correct ("What is the most pressing problem facing the economy? A good case can be made for the developing health care crisis. Soaring costs, growing ranks of uninsured and a steady erosion of corporate health benefits add up to a giant drag on the nation’s future prosperity."), this ought to be domestic policy issue #1 between now and the 2008 elections. But I'm not taking any bets.
CBO and tax-exempt hospitals
 This month the Congressional Budget Office issued two reports on the tax-exempt hospital industry. Both are worth reading, as much for what they say about the mind-set on Capital Hill these days as for what they tell us about tax-exempt hospitals.
This month the Congressional Budget Office issued two reports on the tax-exempt hospital industry. Both are worth reading, as much for what they say about the mind-set on Capital Hill these days as for what they tell us about tax-exempt hospitals.1. Nonprofit Hospitals and the Provision of Community Benefits. How much tax benefit do nonprofit hospitals receive as a result of their exemption from federal, state, and local taxation? Answer (as of 2002): $12.6 billion, about half of which comes from the federal income-tax exemption. And what is the value of the community benefits provided by the tax-exempts? Therein lies a tale, because it all depends on how you define (and measure) community benefits. This report breaks out "uncompensated care" (also a thorny definitional problem), the unreimbursed cost of providing Medicaid-covered services, and such generally unprofitable specialized services as burn intensive care, emergency room care, high-level trauma care, and labor and delivery services. This reports limits itself to five states, including one (Texas) with a very explicit community-benefits requirement for nonprofit hospitals. The tax-exempt hospitals' performance in these three areas of service are also compared to their for-profit and government-owned counterparts. How do they compare?
- When regression techniques were used to adjust for the hospitals’ size and location and for the characteristics of the local populations, nonprofit hospitals were estimated to have an average uncompensated care share that was 0.6 percentage points higher than that for otherwise similar for-profit hospitals. That estimated difference corresponds to nonprofit hospitals in the five selected states providing between $100 million and $700 million more in uncompensated care than would have been provided if they had been for-profits.
- When regression techniques were used to control for hospital characteristics, nonprofit hospitals were found to have adjusted Medicaid shares that were 1.3 percentage points lower than those of otherwise similar for-profit hospitals.
- CBO found that nonprofit hospitals were more likely than for-profit hospitals to provide each of the four specialized services examined. After adjustment for hospital characteristics, nonprofit hospitals were found to be significantly more likely than for-profit hospitals to provide two of the four specialized patient services (emergency room care and labor and delivery services).
2. Nonprofit Hospitals and Tax Arbitrage. This one's a little more technical. It deals with the ability of tax-exempt hospitals to borrow at below-market rates by issuing tax-exempt bonds and then deploy the borrowed funds for higher-yielding investments. So-called "arbitrage bonds," however, are not exempt from federal taxes, which removed the main incentive to engage in such practices. That said, there are plenty of other opportunities for nonprofit hospitals to engage in a sort of tax arbitrage, and this report analyzes some of them. One occurs when a tax-exempt entity decides to invest some of its accumulated surplus and gifts in high-yield taxable securities and to finance structures and equipment with low-cost exempt bonds. In economic terms, it's the same as if bond proceeds were being invested in securities, and there's a "replacement proceeds rule" (26 CFR § 1.148-1(c)) that attempts to identify such events and subject them to taxation. But for a variety of reasons the rule is difficult to apply and undoubtedly misses a lot of such tax-arbitrage activity. The CBO report considers the possibility of broadening the definition of tax arbitrage, which they conclude would probably result in increased tax revenues for the federal government, at least in the short run. But over time, it seems likely hospitals would adjust to the new (increased) cost of capital by reducing their level of arbitrage bond issues, resulting in a decrease in tax savings for the federal government, even under the broader definition. A second likely effect would be
two different costs of capital for nonprofit hospitals. Nonprofits with larger portfolios of investment assets would be more likely to be subject to the rule and thus effectively face higher interest costs associated with financing using taxable debt. Hospitals with smaller amounts of such assets would be more likely to continue to receive the benefit of tax-exempt financing. Both would still face lower costs of capital than for-profit hospitals. But the different borrowing costs of the two groups of nonprofit hospitals could engender inefficiencies by creating a new differential in capital costs.
Saturday, December 30, 2006
Drug wholesaler settles with New York
Thanks to Eric Turkewitz, who "represented a counterfeit drug victim, Tim Fagan, for whom pending legislation in the House and Senate is named," for the heads up. The House and Senate bills are the Counterfeit Drug Enforcement Act of 2005, [H.R.2345.IH], [S.1978.IS].Cardinal -- based in Dublin, Ohio and ranked 19th on the Fortune 500 list of America's largest corporations -- is one of the three primary distributors of prescription drugs in the nation.
In today's settlement, Cardinal has agreed to adopt a set of Wholesaler Safe Product Practices that establish a new standard for the safe trading of pharmaceuticals and point the way forward for an industry that is vital to the health of Americans.
The investigation, which began in 2005 and is continuing with regard to other wholesalers, concerns trading practices in the secondary market for prescription pharmaceuticals. That is the market in which wholesalers trade drugs among themselves, after the drugs are sold by the manufacturer but before they are purchased by a pharmacy, hospital, or other end user. The wholesalers who sell drugs to other wholesalers are called alternate
source vendors.Secondary market trading is not illegal on its face, but can create opportunities for the introduction of unreliable drugs, including counterfeits, into the marketplace. In recent years, there has been an increase in the number of cases of counterfeit drugs in the American supply chain.
Secondary market trading also can create an opportunity for companies to divert drugs from their intended distribution channels. Diversion into the secondary market, often to take improper advantage of manufacturer discounts, can begin a series of trades from wholesaler to wholesaler that makes it difficult to trace the origin of a drug and impossible to ascertain its authenticity.The investigation determined that Cardinal purchased drugs from certain alternate source vendors, despite risks associated with buying from those vendors, to take advantage of higher available profit margins. Cardinal also sold pharmaceuticals to certain customers even in the face of evidence that those customers may have been illegally diverting the drugs outside their intended channels of distribution.
Under the terms of today's settlement, Cardinal will adopt an innovative set of Wholesaler Safe Product Practices, and has agreed that it will not sell pharmaceuticals to another wholesaler unless that wholesaler also adopts that same set of practices. The Wholesaler Safe Product Practices are designed to ensure that a drug may not pass through the hands of more than two wholesalers after the manufacturer sells it and before it is bought by a pharmacy or other end user.In addition to adopting the Wholesaler Safe Product Practices, Cardinal has agreed that in the regular course of its business it will:
- Buy pharmaceuticals directly from manufacturers and not on the secondary market from alternate source vendors;
- Sell pharmaceuticals only to wholesalers who have certified their compliance with the Wholesaler Safe Product Practices, and have agreed to allow audits of those certifications;
- Adopt "know your customer" provisions and monitor for customer diversion; and
- Hire an external auditor to conduct periodic reviews of its compliance with the settlement.
Middlemen redux
 Following up on my earlier post about the role of middlemen in health care, yesterday's WSJ had a nice front-page article (link good for 7 days) on middlemen. After extolling the usual list of the virtues of a middleman --
Following up on my earlier post about the role of middlemen in health care, yesterday's WSJ had a nice front-page article (link good for 7 days) on middlemen. After extolling the usual list of the virtues of a middleman --A lot of the money that goes to health-care middlemen is well spent. It allows employers to combine their purchasing power for leverage with hospitals and drug makers. It harvests data to uncover which new procedures are valuable and which aren't. Middlemen offer health-care expertise to employers who don't have it and don't want to hire it.-- the author then nails the downside:
But a lot of the money goes more toward fattening middlemen's bottom lines than toward improving the quality or efficiency of American health care. "At the end of the day, the only reasonable conclusion is that we waste a huge amount of money on the most nuttily cumbersome administrative system in the world," says Henry Aaron, a Brookings Institution economist.Amen.
When will this madness end?
The full case file for In re Advocate Health Partners et al., No. 0310021, is here. The proposed consent decree is available for public review and comment before the Commission decides whether to make it final.The FTC’s complaint challenges conduct during the period 1995 to 2004, during which the respondents collectively negotiated the prices and other contract terms at which their otherwise competing member physicians would provide services to the subscribers of health plans, without any efficiency-enhancing integration of their practices sufficient to justify their conduct. In particular, for a period of time AHP staff negotiated contracts on behalf of each PHO respondent, with each PHO respondent retaining authority to approve offers and counteroffers.Subsequently, AHP was given the authority to approve offers and counteroffers and, ultimately, to approve negotiated contracts on behalf of the AHP physicians, who could then opt in or out of the negotiated contract.
The complaint also alleges that in 2001, AHP terminated its members’ contracts with a health plan that rejected contract proposals for higher fees, and threatened that it would not contract with the plan for hospital services unless it stopped contracting with individual physicians and agreed to a group contract. The resulting contract included fees 20 percent to 30percent higher than the health plan’s individual physician contracts.
This is, by my rough count, the 22nd price-fixing/boycott case brought against physicians and/or physician groups or their representatives by the FTC since 2002 for similar or in some cases identical conduct. You can read all about them in the useful "Overview of FTC Antitrust Actions in Health Care Services and Products (Aug. 2006)."
The spine as profit center
 Today there is yet another story from The New York Times about yet another opportunity for entrepreneurial docs (this time, spine surgeons) to combine with entrepreneurial manufacturers (this time, of medical devices) for mutual profit. Not, as Jerry used to say, there is anything wrong with that, unless the profit motive is warping medical judgment and leading surgeons to make decisions based upon the impact on their investment in the company that manufactures the medical devices to the detriment of their patients. There are medical-malpractice implications, of course, but there are also signs that federal regulators are concerned about fraud an abuse (antikickback, 42 USC § 1320a-7b(b)), as well as an emerging body of professional ethical opinion that the inherent conflict of interest is not defensible:
Today there is yet another story from The New York Times about yet another opportunity for entrepreneurial docs (this time, spine surgeons) to combine with entrepreneurial manufacturers (this time, of medical devices) for mutual profit. Not, as Jerry used to say, there is anything wrong with that, unless the profit motive is warping medical judgment and leading surgeons to make decisions based upon the impact on their investment in the company that manufactures the medical devices to the detriment of their patients. There are medical-malpractice implications, of course, but there are also signs that federal regulators are concerned about fraud an abuse (antikickback, 42 USC § 1320a-7b(b)), as well as an emerging body of professional ethical opinion that the inherent conflict of interest is not defensible:Spinal-fusion surgery is one of the most lucrative areas of medicine. An estimated half-million Americans had the operation this year, generating billions of dollars for hospitals and doctors.
But there have been serious questions about how much the surgery actually helps patients with back pain and whether surgeons’ generous fees might motivate them to overuse the procedure. Those concerns are now heightened by a growing trend among some surgeons to profit in yet another way — by investing in companies that make screws and other hardware they install.
The parts can be highly profitable. A single screw that goes into the spine, for example, sells for about $1,000 — at least 10 times the cost of making it.
Within the medical device industry, it has been well chronicled how companies use consulting ties and other financial relationships to try to gain favor with the surgeons using their devices. But critics are especially troubled by the emerging trend in spinal devices, which so far has occurred largely under the radar.
Doctors’ taking significant ownership stakes in spinal parts makers, critics say, provides an extra financial incentive for a doctor to recommend a surgery. It may be one of the most distinct examples yet of the way monetary considerations can play a role in the way doctors practice medicine.
Such doctors face “an awfully pernicious conflict of interest,” said Dr. Richard A. Deyo, a physician and health services professor at the University of Washington in Seattle.
About 30 start-up companies have begun selling spinal devices, including screws, in the last couple of years. And industry experts say about a dozen companies have doctors among their investors. Because most of the companies are private and the relationships are not publicly disclosed, there is no way to know how many spine surgeons around the country are partial owners of device makers.
Typically, patients are not aware of the doctor’s financial interests. One patient who is suing her surgeon for malpractice learned only during the legal discovery process that her surgeon had a financial interest in the maker of the artificial disk he installed in her spine.
Federal regulators have voiced concerns about the growing popularity of the investment arrangements, which would potentially violate antikickback laws if doctors receive stock or are otherwise compensated to use or recommend certain devices.
“This is an area that is new and growing,” Vicki L. Robinson, a senior attorney in the Office of Inspector General at the Department of Health and Human Services, said in an interview. In a recent letter to a device industry trade group, Ms. Robinson wrote that the “ventures should be closely scrutinized under the fraud and abuse laws.”
Some spine surgeons are also concerned about whether they and their colleagues should enter into such arrangements. “These are, I believe, unethical and bias the doctors’ choice for what is best for the patient,” said Dr. Charles D. Rosen, a spine surgeon at the University of California at Irvine, who is the president of the newly formed Association of Ethical Spine Surgeons. The group has about 75 members so far, who have agreed not to invest in companies whose devices they use.
Other articles in the Times' series ("Side Effects"), which "examin[es] how monetary considerations can influence the ways doctors conduct business and practice medicine," include:
- Profit and Questions on Prostate Cancer Therapy (Dec. 1, 2006)
- New Nerve Test, a Moneymaker, Divides Doctors (Oct. 20, 2006)
- Heart Procedure Is Off the Charts in an Ohio City (Aug. 18, 2006)
- Drug Makers Pay for Lunch as They Pitch (July 28, 2006)
- Indictment of Doctor Tests Drug Marketing Rules (July 22, 2006)
- Charities Tied to Doctors Get Drug Industry Gifts (June 28, 2006)
Thursday, December 28, 2006
Viaticals -- something was rotten, indeed
 From today's Modern Healthcare "Daily Dose":
From today's Modern Healthcare "Daily Dose":Florida physician Clark Mitchell pleaded guilty to participating in a securities fraud scheme with Mutual Benefits Corp. that robbed investors of $965 million and conspiracy to commit healthcare fraud. According to the U.S. attorney's office for the Southern District of Florida, MBC principals induced investors to purchase interests in the life-insurance-policy death benefits of terminally ill or elderly people in return for a lump-sum cash payment. MBC dictated fraudulently low life-expectancy figures on thousands of the policies to doctors including Mitchell, who signed more than 5,000 letters and affidavits to investors falsely claiming that a physician completed a review of the insured's medical condition to determine life expectancy. Mitchell also pleaded guilty to inflating Medicare bills by more than $500,000 while he was director of an AIDS clinic. Mitchell will be responsible for $367 million in restitution payable to MBC investors and $500,000 in restitution for the healthcare fraud. He also faces up to 10 years in prison and a $5 million fine. His sentencing is scheduled for March 7, 2007.The Orlando Sentinel has a good story on this case.
For years, I had been skeptical of these contracts, but my concern had to do with the potential for coercive deals with dying patients who had run out of financial options and signed over life insurance contracts out of desperation and on terms that bordered on the unconscionable. Occasionally, the premiums for these policies had been paid by partners while they were still healthy enough to work and who could find themselves with nothing after the death of the insured person. I hadn't thought about the potential for ripping off investors, so a tip of the hat to Dr. Mitchell, whose breathtakingly massive fraud adds a chapter to my education on the subject of viaticals.
DeBakey's surgery
 It is sometimes said you should be able to teach an entire Bioethics course from the stories that appear in your local daily paper, but it is also sometimes the case that you could teach the course from a single article. Once such article is "The Man on the Table Devised the Surgery" in the Christmas-day edition of The New York Times.
It is sometimes said you should be able to teach an entire Bioethics course from the stories that appear in your local daily paper, but it is also sometimes the case that you could teach the course from a single article. Once such article is "The Man on the Table Devised the Surgery" in the Christmas-day edition of The New York Times.The gist of the story is pretty straightforward. Last Dec. 31, DeBakey, then 97 years old, was working at home
His heart didn't stop, and his self-diagnosis shifted to another life-threatening condition, a dissecting aortic aneurysm. Ironically, he pioneered the surgical procedure for correcting such conditions. Now, it appeared, he would have his own procedure performed on himself. And, one year later, he is the oldest patient ever to survive the procedure.when a sharp pain ripped through his upper chest and between his shoulder blades, then moved into his neck.
Dr. DeBakey, one of the most influential heart surgeons in history, assumed his heart would stop in a few seconds.
“It never occurred to me to call 911 or my physician,” Dr. DeBakey said, adding: “As foolish as it may appear, you are, in a sense, a prisoner of the pain, which was intolerable. You’re thinking, What could I do to relieve myself of it. If it becomes intense enough, you’re perfectly willing to accept cardiac arrest as a possible way of getting rid of the pain.”
Nice story, but that's not the end of it. Lawrence Altman is too good a doctor and too experienced a medical journalist not to notice the other strands of this tale:
[B]eyond the medical advances, Dr. DeBakey’s story is emblematic of the difficulties that often accompany care at the end of life. It is a story of debates over how far to go in treating someone so old, late-night disputes among specialists about what the patient would want, and risky decisions that, while still being argued over, clearly saved Dr. DeBakey’s life.
It is also a story of Dr. DeBakey himself, a strong-willed pioneer who at one point was willing to die, concedes he was at times in denial about how sick he was and is now plowing into life with as much zest and verve as ever.
Consider:
- DeBakey himself did not want the operation. He did not check into the hospital for nearly a month. After he did, he had a DNR order on his chart and a progress note that indicated he did not want surgery for the dissecting aortic aneurysm. How, then, did he get the surgery (and the continuous resuscitation that went along with the surgery), apparently against his wishes? (And would the result have been any different if he had executed an advance directive that forbade surgery?)
- The hospital ethics committee got involved. The question was apparently whether to follow DeBakey's stated wishes or the contrary instructions of his spouse. Lay people are often surprised that family members are taken seriously when they attempt to override a patient's medical choices, but they are, often to the point of an ethics consult to try to reconcile the family to the patient's wishes. This time, the ethics committee decided the spouse's wishes should prevail. Altman doesn't report their reasons, but the outcome ran against his reported preferences. As Altman reports, "Dr. DeBakey says that he refused admission to Methodist Hospital, in part because he did not want to be confined and he 'was hopeful that this was not as bad as I first thought.' He feared the operation that he had developed to treat this condition might, at his age, leave him mentally or physically crippled. 'I’d rather die,' he said."
These are usually decisions we allow a competent patient to make for himself. The flip side of the coin, however, is that once he was admitted, and after his condition worsened and his doctors recommended surgery, he said he wanted to re-evaluate the situation in a couple of days, which certainly suggests that he was willing to depart from the "no surgery" position he took at the time of his admission. Also, Altman reports:Each of Dr. DeBakey’s doctors had worked with him for more than 20 years. One, Dr. Pool, said they felt they knew Dr. DeBakey well enough to answer another crucial question from the ethics committee: As his physicians, what did they believe he would choose for himself in such a dire circumstance if he had the ability to make that decision?
DeBakey's condition continued to deteriorate, though, and he became unresponsive and was close to death before he could make his "re-evaluation." Under those circumstances, and with a life hanging in the balance, it was proper for the hospital's ethics committee to convene to decide whether there was sufficient evidence that he might have agreed to the operation to justify ignoring his prior statements.
Dr. Noon said that Dr. DeBakey had told him it was time for nature to take its course, but also told him that the doctors had “to do what we need to do.” Members of Dr. DeBakey’s medical team said they interpreted the statements differently. Some thought he meant that they should do watchful waiting, acting only if conditions warranted; others thought it meant he wanted to die. - The home care he received for three weeks, with occasional trips to the hospital for imaging to measure the size of the aneurysm, was a departure from the standard of care: "In providing the extraordinary home care, the doctors were respecting the wishes of Dr. DeBakey and their actions reflected their awe of his power." VIP medicine is usually discussed in medical school as a risk -- it often involves departures from standards and procedures that work far more often than not. VIP medicine, contrary to its connotation, is not usually better medicine but just the opposite. In DeBakey's case, it sounds as though he got a pretty high level of "home care" and that it was far from suboptimal. Still, time and distance would have separated his home from the operating room had he needed a procedure on an emergent basis, an increased risk that resulted from his insistence that he not be admitted and his doctors' decision to acquiesce to a preference other, less fearsome patients would not have been allowed to make.
- None of the anesthesiologists at Methodist Hospital were willing to participate in the surgery in light of his age and condition. Eventually an anesthesiologist from a different hospital put him to sleep. I've always marveled at the ability of surgeons and, in this case, anesthesiologists to unilateral refuse to perform a procedure when they think a patient is not a candidate for surgery. When did they acquire this right? When did medical docs lose it? The chancellor of the medical center is reported to have been stunned by their decision, one that he says he had never heard of before. (I'm stunned that he was stunned.) What does seem stunning, though, was the reported fact that none of the demurring anesthesiologists had been involved in his care so far and none had reviewed his medical record, so that their refusal was based upon "grapevine information." Maybe all they thought they needed to know was that the patient was 97 years old and on death's doorstep to conclude that his post-surgical prognosis, even with the best of care, was dismal. And maybe they would have had more going for their conclusion if they had reviewed his records before refusing.
Other interesting questions arose. As reported by Dr. Altman, the "other anesthesiologist" was Dr. Salwa Shenaq from the Michael E. DeBakey Veteran Affairs Medical Center, who had worked with Dr. DeBakey for 22 years:She said that a medical staff officer, whom she declined to name, warned her that she could be charged with assault if she touched Dr. DeBakey. The officer also told Dr. Shenaq that she could not give Dr. DeBakey anesthesia because she did not have Methodist Hospital privileges. She made it clear that she did, she said.
- The cost of his care "easily exceeded $1 million," and neither the hospital nor the physicians involved paid for his care. Professional courtesy? Who benefited from the professional courtesy? His insurer, probably. Who paid? Everyone else who paid for care at the hospital, through the increasingly difficult phenomenon of cross-subsidization, and others who might have benefited from alternative uses of that money, to the extent it came off Methodist's bottom line.
- Ethics committees spend a lot of time trying to divine patients' wishes. State laws require that very serious consideration be given to formal expressions of a patient's treatment and nontreatment preferences, with penalties for failing to do so. And yet, as the academic literature occasionally points out, patients' actual preferences frequently depart from their prior statements. That seems to be exactly the situation with Dr. DeBakey:
As he recovered and Dr. DeBakey learned what had happened, he told his doctors he was happy they had operated on him. The doctors say they were relieved because they had feared he regretted their decision.
“If they hadn’t done it, I’d be dead,” he said.
The doctors and family had rolled the dice and won.
Dr. DeBakey does not remember signing an order saying not to resuscitate him and now thinks the doctors did the right thing.
Doctors, he said, should be able to make decisions in such cases, without committees.
Wednesday, December 27, 2006
Physicians' "verbal orders": who may authenticate them?
 It probably isn't worth fighting this fight, so I won't, but I have to note in passing that all physicians' orders are verbal orders as long as they used words in some form or another (either written or oral), which pretty much includes everything except body language. (See, e.g., Columbia Guide to Standard American English.) But, by long-standing practice, "verbal orders" is the established phrase for orders that are spoken by the physician, typically over the telephone.
It probably isn't worth fighting this fight, so I won't, but I have to note in passing that all physicians' orders are verbal orders as long as they used words in some form or another (either written or oral), which pretty much includes everything except body language. (See, e.g., Columbia Guide to Standard American English.) But, by long-standing practice, "verbal orders" is the established phrase for orders that are spoken by the physician, typically over the telephone.Now that the usage lesson is over, the really interesting development with verbal orders is CMS' revision this fall to the Medicare Conditions of Participation:
In a surprising development, the newly revised Medicare conditions of participation (CoP) allow nurse practitioners and physician assistants to authenticate physicians' verbal orders, says Houston attorney Nancy LeGros. The Nov. 27 final CoP regulation said that verbal orders must be signed, dated and authenticated by the ordering physician — or another practitioner responsible for the patient's care — within 48 hours. CMS stated that physician extenders can authenticate physician orders as long as physician extenders are licensed to perform the services included in the verbal order, says LeGros, who is with the law firm of Vinson & Elkins.
This tidbit came from the Dec. 18, 2006, issue of Report on Medicare Compliance. The final rule appeared in the Nov. 27 Federal Register and included this language in the Preamble (at pp. 68682-83):
Comment: One commenter requested clarification as to whether a physician assistant or nurse practitioner who has prescriptive authority under State law is allowed to co-sign a physician's order.
Response: A physician assistant or nurse practitioner may only authenticate verbal orders written by a physician or other licensed independent practitioner that they have authority to write themselves as determined by hospital policy in accordance with state law. For example, some hospitals limit who may give orders for certain types of drugs or therapies. If a physician assistant or nurse practitioner is not permitted by hospital policy to order a specific drug or therapy, he or she would not be permitted to authenticate a verbal order for such a drug or therapy. Hospitals have the flexibility to limit who may authenticate verbal orders.In addition, a physician assistant or nurse practitioner may only authenticate verbal orders for a patient for whom they have physician delegated responsibility. Like all practitioners responsible for the care of the patient, a physician assistant or nurse[[Page 68683]]practitioner would be expected to have knowledge of the patient's hospital course, medical plan of care, condition and current status. With this knowledge, a practitioner can safely evaluate the completeness and accuracy of a verbal order.
Nice news for the antitrust bar
 Worth watching in 2007:
Worth watching in 2007:Nurses filed a class-action antitrust lawsuit against Detroit-area hospitals and health systems, claiming that they colluded since before November 2002 to fix wages at below-market levels. The lawsuit, filed in U.S. District Court in Detroit, names Bon Secours Cottage Health Services, Detroit Medical Center, Henry Ford Health System, McLaren Health Care Corp., Oakwood Healthcare and St. John Health Partners. It follows similar class actions filed on behalf of nurses in Arizona, Illinois, New York, Tennessee and Texas. A spokesman for the Michigan Health & Hospital Association declined to comment on the matter, citing the pending litigation.
[Modern Healthcare's "Daily Dose" (time-limited link)]
What ever happened to the bird flu pandemic?
 AP ran a story this month ("Experts Puzzle Over Halt of Bird Flu") with a couple of interesting points:
AP ran a story this month ("Experts Puzzle Over Halt of Bird Flu") with a couple of interesting points:- Bird flu may not be gone, but merely resting -- there are lots of potential hiding places, made difficult to find because of a combination of factors, including warmer weather, poultry vaccination programs, and the reluctance of academics and developing countries to part with virus samples.
- Cold weather, which allows the virus to live longer, encourages the spread of flu, and winter weather is just around the corner.
- It's way too early for public health authorities to breathe a sigh of relief.
Tuesday, December 26, 2006
Talking about what doctors don't want to talk about
 Death.
Death.Today's New York Times has an op-ed by Dr. Pauline Chen on "The Most-Avoided Conversation in Medicine" -- i.e., the one that includes the words "you're dying and we've run out of ways to slow it or stop it." Chen's useful suggestion, which probably amount to spitting into the wind but is worth repeating to every medical student and doctor you meet: "I think there is a simple way to change. We could add one question to every discussion we have about patients with terminal illnesses: 'How good is this patient’s end-of-life care?'” In conclusion:
Anyone interested in pursuing this topic further should pick up a copy of the Nov. 15, 2000 (!) issue of JAMA, which was dedicated to End-of-Life Care and included a valuable piece by Dr. Tim Quill, "Initiating End-of-Life Discussions With Seriously Ill Patients: Addressing the 'Elephant in the Room.'"The forums for posing this question are plentiful in medicine. Every morning and late afternoon, physicians in hospitals “round” on their patients, discussing their decisions in small groups or writing progress notes on patients’ charts. Doctors hold “grand rounds” (lectures before their colleagues) monthly or weekly, and in academic centers, physicians hold regular teaching conferences.
If in these settings we could bring ourselves to ask about each patient’s end-of-life care, we could influence one another in a more personal way than the Support study did. And while we might not get all the details right at first, we would grow more familiar with advance directives and pain treatment and learn to manage our patients’ resuscitation wishes.
We also might find ourselves — as I have found myself with patients since J. R. — one step closer to being the compassionate doctors we have always dreamed of becoming.
Saturday, December 23, 2006
The Willie Sutton School of Healthcare Cost Management
 Considering the incredible profits being earned by many of the middlemen in the health care industry, wouldn't you think there would be a more efficient way to deliver health care that didn't require the services of the paper-pushers, leaving more money on the table for goods and services that actually benefit real patients? That was one of the lessons, I thought, from the story involving United Healthcare and its CEO, Dr. Bill McGuire, whose compensation was in the billions (when you include ill-gotten gains on back-dated stock options). (Saul Friedman at Newsday.com, for one, sees it my way.)
Considering the incredible profits being earned by many of the middlemen in the health care industry, wouldn't you think there would be a more efficient way to deliver health care that didn't require the services of the paper-pushers, leaving more money on the table for goods and services that actually benefit real patients? That was one of the lessons, I thought, from the story involving United Healthcare and its CEO, Dr. Bill McGuire, whose compensation was in the billions (when you include ill-gotten gains on back-dated stock options). (Saul Friedman at Newsday.com, for one, sees it my way.)The case for a system that doesn't depend on middlemen -- or that at least doesn't create billions in profits for the paper-pushers in the system -- is even more compelling when the middleman is working overtime on schemes to keep our costs and its profits high, despite actions by payors that are designed to cut costs without cutting quality or access to care. For example, in today's Wall Street Journal, there's a report [link good for a week] on Omnicare, a large operator of pharmacies and provider of pharmacy-related services for seniors. Seems they were switching patients to Zantac capsules just as Medicaid was slashing its reimbursement for Zantac tablets:
Last month, Omnicare reached a $49.5 million settlement with 42 states and the federal government over allegations about dosage switches for generic Zantac and two other drugs. Omnicare agreed in October to pay $52.5 million to the state of Michigan over separate accusations of Medicaid overbilling. Omnicare didn't admit wrongdoing as part of the settlements.
Friday, December 22, 2006
Some folks have a head for business . . . .
 The AP reports (courtesy of MyWay) on an interesting case that lies at the intersection of criminal procedure and a patient's right to refuse an unwanted medical procedure. Seventeen-year-old Joshua Bush has a 9mm bullet in his head. Its presence isn't life-threatening, and a procedure to remove it wouldn't be any more dangerous than other surgeries that require general anesthesia. He has refused requests to have it removed, and is resisting a subpoena to obtain the bullet, presumably because it may link him to a robbery of a used car lot in which shots were exchanged. So who will win? The state, which has an interest in seeing an alleged shooter brought to justice? Or a person of interest to law-enforcement who would rather not have doctors poking around his head? Art Caplan says he thinks Bush will win. More on this later . . . . (Thanks to Maguire Center Coordinator Terri Gwinn for the tip.)
The AP reports (courtesy of MyWay) on an interesting case that lies at the intersection of criminal procedure and a patient's right to refuse an unwanted medical procedure. Seventeen-year-old Joshua Bush has a 9mm bullet in his head. Its presence isn't life-threatening, and a procedure to remove it wouldn't be any more dangerous than other surgeries that require general anesthesia. He has refused requests to have it removed, and is resisting a subpoena to obtain the bullet, presumably because it may link him to a robbery of a used car lot in which shots were exchanged. So who will win? The state, which has an interest in seeing an alleged shooter brought to justice? Or a person of interest to law-enforcement who would rather not have doctors poking around his head? Art Caplan says he thinks Bush will win. More on this later . . . . (Thanks to Maguire Center Coordinator Terri Gwinn for the tip.)
Piergiorgio Welby dies after respirator removed
 The Italian poet who lost in his bid for court authorization to have his respirator removed (see earlier post), died after his physician removed the respirator without official permission (Reuters). Meanwhile, AP reports that prosecutors in Rome are looking into the details of Welby's death (AP/CBS News).
The Italian poet who lost in his bid for court authorization to have his respirator removed (see earlier post), died after his physician removed the respirator without official permission (Reuters). Meanwhile, AP reports that prosecutors in Rome are looking into the details of Welby's death (AP/CBS News).The death came the evening after an expert medical panel ruled Wednesday "that the use of a mechanical respirator 'does not constitute, as of now, extraordinary means.' But the panel also decided that precise guidelines for doctors were needed urgently to spell out what the law allows and what it does not" (International Herald Tribune). The Roman Catholic Curch in Italy has apparently already reached its own conclusions about Welby's death and earlier today denied his family's request for a church funeral (Reuters).
Wednesday, December 20, 2006
Italian poet pushes the law on his right to die
 Today's New York Times has a story about Piergiorgio Welby, an Italian poet who apparently has entered the final chapter in his 40-year fight with muscular dystrophy. His breathing is supported by a respirator and he may have a feeding tube (the article isn't crystal clear on this point), and he has asked for permission to have his respirator removed. Italian authorities have so far said no:
Today's New York Times has a story about Piergiorgio Welby, an Italian poet who apparently has entered the final chapter in his 40-year fight with muscular dystrophy. His breathing is supported by a respirator and he may have a feeding tube (the article isn't crystal clear on this point), and he has asked for permission to have his respirator removed. Italian authorities have so far said no:The article says that Italian law allows patients to refuse unwanted medical treatments but is unclear as to the right of a physician to participate. That's confusing enough, but what the article says about the Catholic Church's position in this case is more so:“I love life, Mr. President,” Mr. Welby, 60, who has battled muscular dystrophy for 40 years, wrote to Italy’s president, Giorgio Napolitano, in September. “Life is the woman who loves you, the wind through your hair, the sun on your face, an evening stroll with a friend.
“Life is also a woman who leaves you, a rainy day, a friend who deceives you. I am neither melancholic nor manic-depressive. I find the idea of dying horrible. But what is left to me is no longer a life.”
Now Mr. Welby’s long drama appears to be nearing its final act. Last weekend, an Italian court denied legal permission for a doctor to sedate him and remove him from his respirator. Fully lucid but losing his capacity to speak and eat, he is deciding whether to appeal or to perform an act of civil disobedience that will kill him.
The church, too, has conflicting teachings about what to do in this case, and what the Vatican thinks has a deep impact not only on the nation’s political class but also on doctors tied to the scores of Catholic-run hospitals around Italy.I had thought that the Catholic Church had long ago accepted that patients could refuse "extraordinary" treatments, even life-sustaining ones, and that one of the defining notions behind "extraordinary" is that the treatment merely prolongs the dying process. Granted, "prolongation" may be in the eye of the beholder, but Welby's death appears to be reasonably imminent with or without life-supporting measures and so it should be a relatively easy one for Church leaders. Or am I missing something?
The defense of life is central to the social doctrine of the church, and so it opposes abortion and capital punishment. Only last week Pope Benedict XVI reaffirmed his opposition to euthanasia, saying governments should find ways to let the terminally ill “face death with dignity.”
The church also opposes medical treatments to artificially prolong life, but several church officials have worried recently that ending artificial life support could result in de facto euthanasia.
“The problem is to know if we find ourselves truly in front of a case of an artificial prolonging of life,” Cardinal Javier Lozano Barragán, the Vatican’s top official for health, said in a recent interview with La Repubblica.
Links for more information about this case:
- BBC article with useful links to related stories
- Pope Benedict XVI's Dec. 8 remarks about caring for the incurably ill
Tuesday, November 14, 2006
Federal pre-emption of state-law claims medical-device manufacturers
 This issue keeps turning up on SCOTUS' docket every few years like the proverbial bad penny. Most recently, it takes the form of Riegel v. Medtronic, No. 06-179. The petition for certiorari to the Second Circuit is pending, and after it was considered by the Court at its Nov. 3 conference, the justices invited the Solicitor General's office (on Nov. 6) to file a brief addressing the cert-worthiness of the case (known in the parlance of the trade -- the Supreme Court advocacy trade, that is -- as a CVSG (a "call for the views of the Solicitor General"). When the SG's brief is filed, it will be posted here. Thanks to Aaron Streett's excellent (and wickedly irreverent) Supreme Court e-mail newsletter for this bit of intelligence (subscription requests to "SCt Today" may be sent here).
This issue keeps turning up on SCOTUS' docket every few years like the proverbial bad penny. Most recently, it takes the form of Riegel v. Medtronic, No. 06-179. The petition for certiorari to the Second Circuit is pending, and after it was considered by the Court at its Nov. 3 conference, the justices invited the Solicitor General's office (on Nov. 6) to file a brief addressing the cert-worthiness of the case (known in the parlance of the trade -- the Supreme Court advocacy trade, that is -- as a CVSG (a "call for the views of the Solicitor General"). When the SG's brief is filed, it will be posted here. Thanks to Aaron Streett's excellent (and wickedly irreverent) Supreme Court e-mail newsletter for this bit of intelligence (subscription requests to "SCt Today" may be sent here).The opening paragraphs of the Second Circuit's 2-1 opinion tell the tale nicely:
So there is a slight split in the circuits, more of a fissure, really, and the Court has asked the SG's office to offer some guidance on the need for the Court to clear up the confusion (whichever side might be said to be confused). Stay tuned . . . .This case calls upon us to determine, inter alia, the scope of the preemption provision set forth in Section 360k(a) of the 1976 Medical Device Amendments to the Food, Drug, and Cosmetic Act, 21 U.S.C. §§ 301 et. [sic] seq. [link]Specifically, we must decide whether Section 360k(a) preempts common law tort claims regarding medical devices that have entered the market pursuant to the Food and Drug Administration’s (“FDA”) rigorous premarket approval (“PMA”) process. The Supreme Court left open this question in Medtronic v. Lohr, 518 U.S. 470 (1996) [link], which held that tort claims as to medical devices that have entered the market pursuant to the far less intensive premarket notification process (often referred to as the “Section 510(k) process”) are not preempted by Section 360(k)(a) [sic]. Since Lohr, the majority of circuits addressing this question have held that claims regarding PMA-approved medical devices are, by contrast, preempted. See Horn v. Thoratec Corp., 376 F.3d 163 (3d Cir. 2004); Martin v. Medtronic, Inc., 254 F.3d 573 (5th Cir. 2001); Brooks v. Howmedica, Inc., 273 F.3d 785 (8th Cir. 2001); Kemp v. Medtronic, Inc., 231 F.3d 216 (6th Cir. 2000); Mitchell v. Collagen Corp., 126 F.3d 902 (7th Cir. 1997); but see Goodlin v. Medtronic, Inc., 167 F.3d 1367 (11th Cir. 1999).
We now join this growing consensus and hold that tort claims that allege liability as to a PMA-approved medical device, notwithstanding that device’s adherence to the standards upon which it obtained premarket approval from the FDA, are preempted by Section 360(k)(a)[sic]. . . .
It's been a long time . . .
 of a long time since my last post, due mostly to conferences and speeches the past few weeks at the Maguire Center for Ethics, combined with some speechifying of my own, on top of teaching, cranking out a new poetry column for the Dallas Morning News (scheduled for this Sunday's paper), and a few other official chores PLUS
of a long time since my last post, due mostly to conferences and speeches the past few weeks at the Maguire Center for Ethics, combined with some speechifying of my own, on top of teaching, cranking out a new poetry column for the Dallas Morning News (scheduled for this Sunday's paper), and a few other official chores PLUS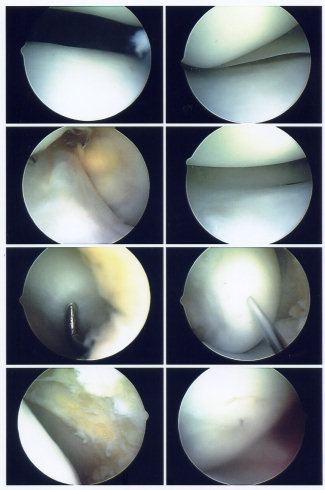 (arthroscopic surgery on a torn medial meniscus) . . . .okay, okay -- too much information. Well, I'm back, at least until we leave for Paris to visit #3 son (with #2 son in tow) next week, which means this page will be down for about 5 days starting
(arthroscopic surgery on a torn medial meniscus) . . . .okay, okay -- too much information. Well, I'm back, at least until we leave for Paris to visit #3 son (with #2 son in tow) next week, which means this page will be down for about 5 days starting Nov. 23. For now -- For a day or two, I'll be playing a little catch-up ball to get through the backlog of interesting or useful (and in some case, useful and interesting) stuff. Stay tuned . . . .
Nov. 23. For now -- For a day or two, I'll be playing a little catch-up ball to get through the backlog of interesting or useful (and in some case, useful and interesting) stuff. Stay tuned . . . .
Tuesday, October 24, 2006
Bones and tissue stolen by undertakers and sold illegally
 This CNN story is just the latest in a long line of exposés of the apparently irremediably corrupt bones-and-tissue market. How long can this business go without significant regulation? USA Today had a good report on the situation in June 2006. The illustration to the right, by the way, shows an X-ray of a corpse whose leg bones were surreptitiously removed and replaced with household PVC pipe, as reported in the CNN story.
This CNN story is just the latest in a long line of exposés of the apparently irremediably corrupt bones-and-tissue market. How long can this business go without significant regulation? USA Today had a good report on the situation in June 2006. The illustration to the right, by the way, shows an X-ray of a corpse whose leg bones were surreptitiously removed and replaced with household PVC pipe, as reported in the CNN story.
Monday, October 23, 2006
Porter & Teisberg's "Redefining Health Care" gets raked over the coals
 I was impressed by Michael Porter's and Elizabeth Olmstead Teisberg's article-length adaption of their health-care policy book when the article appeared in the June 2004 issue of the Harvard Business Review. Now the book is out, and judging from the lukewarm (at best) response over on the Health Affairs blog, it is either not up to the standards one might expect from one of Harvard's 21 University Professors or exactly what you'd expect from a really bright guy who's long on theory and short on real-world health-care experience.
I was impressed by Michael Porter's and Elizabeth Olmstead Teisberg's article-length adaption of their health-care policy book when the article appeared in the June 2004 issue of the Harvard Business Review. Now the book is out, and judging from the lukewarm (at best) response over on the Health Affairs blog, it is either not up to the standards one might expect from one of Harvard's 21 University Professors or exactly what you'd expect from a really bright guy who's long on theory and short on real-world health-care experience.The blog entries are all listed here and include commentary from Gail Wilensky, Alan Maynard, Alan Enthoven, Uwe Reinhardt, and a slightly more upbeat James C. Robinson. Health Affairs' review of the Porter & Teisberg tome (wirtten by Tom Miller) is here.