Health care law (including regulatory and compliance issues, public health law, medical ethics, and life sciences), with digressions into constitutional law, statutory interpretation, poetry, and other things that matter
Thursday, July 01, 2021
CMS Proposes Final Interim Rule to Implement the No Surprises Act
Grand Jury Declines to Indict Houston Doctor Accused of Stealing COVID Vaccine
- The doses were about to be destroyed due to nonuse and aging.
- It was his duty as a physician -- and one employed by the Harris County health department -- to maximize health and protect life.
- Allowing the doses to be destroyed would have been a violation of his professional duties and sacred oath.
Tuesday, June 29, 2021
Hospitals Now Employ 50% of all U.S. Physicians
Once upon a time, it was a virtually universal no-no for a corporation or other lay entity or person to own, or even have an ownership interest in, a physician's practice. There were various rationales for the so-called "corporate practice prohibition," including:
- only natural persons could meet the requirements for medical licensure,which ruled out corporations, trusts, partnerships, etc.
- a corporate or other lay owner created at least the potential for dual loyalties, putting doctors in the impossible position of choosing between his or her patient and corporate overlords; and
- allowing non-physicians to get in on a medical practice's action represented an unseemly commercialization of medical practice.
Thursday, June 17, 2021
SCOTUS Rejects Red States' Challenge to ACA
In a 7-2 decision (majority opinion by Justice Breyer, dissent by Justice Alito), the Supreme Court today tossed out the suit filed by Texas plus other states and two individuals, not on the merits but for lack of standing.
Basic standing analysis requires a direct harm to the plaintiff that is [1] traceable to an unlawful action or provision of law and is [2] redressable if a court were to give the plaintiff the relief it seeks. The majority opinion concluded that -- even if it agreed that the individual mandate lost its constitutional moorings when in 2017 Congress zeroed out the tax for noncompliance -- the only burdens (i.e., "harms") the plaintiffs could point to were the costs of complying with the presumptively lawful parts of the ACA that remained on the books. It is hard to see how future plaintiffs would be able to overcome the standing hurdle created by this opinion.
As the dissent points out,
Today’s decision is the third installment in our epic Affordable Care Act trilogy, and it follows the same pattern as installments one and two. In all three episodes, with the Affordable Care Act facing a serious threat, the Court has pulled off an improbable rescue.
None of this is to say that challenges to the ACA on other grounds can't or won't be brought, but opponents are running out of constitutional theories. Indeed, the Court has already granted cert. in two ACA cases for the 2021 Term (Nos. 20-429 and 20-539), and there are 6 more ACA cases listed for the Court's next conference. See Nos. 20-219, 20-1162, 20-1200, 20-1374, 20-1432, and 20-1536. All 8 cases are statutory-interpretation cases and none challenge the constitutionality of the ACA or any part of it.
Wednesday, June 16, 2021
Surprise billing: It's still a thing
From the Kaiser Family Foundation's news service:
In Alleged Health Care ‘Money Grab,’ Nation’s Largest Hospital Chain Cashes In on Trauma Centers
After falling from a ladder and cutting his arm, Ed Knight said, he found himself at Richmond, Virginia’s Chippenham Hospital surrounded by nearly a dozen doctors, nurses and technicians — its crack “trauma team” charged with saving the most badly hurt victims of accidents and assaults. But Knight’s wound, while requiring about 30 stitches, wasn’t life-threatening. Hospital records called it “mild.” Nevertheless, Chippenham, owned by for-profit chain HCA Healthcare, included a $17,000 trauma team “activation” fee on Knight’s bill, which totaled $52,238 and included three CT scans billed at $14,000. His care should have cost closer to $3,500 total, according to a claims consultant which analyzed the charges for KHN. (KHN, Richmond Times-Dispatch)
The federal No Surprises Act (signed Dec. 27, 2020) was supposed to curb billing abuses. The KHN link has an exhaustive analysis of the problem, but it doesn't say whether Mr. Knight's trip to the ER was before or after the effective date of the new law. (And the Richmond Times-Dispatch link didn't work for me; I've included it here in case it works for you.)
Monday, June 14, 2021
Public Health: The Neglected Infrastructure Crisis
Dr. Anne Schuchat's June 10th NY Times op-ed is a must-read for any and all who want to understand the importance of investment in public health resources as part of our renewed interest in rebuilding the nation's infrastructure. Published upon the eve of her retirement as second-in-command at the CDC after 33 years of public service. It's a great essay that celebrates public service as a career path. It's also a scary-as-hell depiction of the sorry state of public health in this country. Here's an example:
The Covid-19 pandemic is not the first time the U.S. public health system has had to surge well beyond its capacity, but with the worst pandemic in a century and, initially, a heavily partisan political context, the virus collided with a system suffering from decades of underinvestment. A recent report from the National Academy of Medicine revealed that state and local public health departments have lost an estimated 66,000 jobs since around 2008. [emphasis added]
We cannot count on a once-in-a-century cycle of pandemics. There is every reason to believe that all countries -- the more economically developed chief among them -- are susceptible to increasingly frequent outbreaks.
It's time to wake up and get prepared for when not if.
Wednesday, May 26, 2021
SCOTUS still has to decide a big ACA case
I have a hard time believing the Court will affirm the Fifth Circuit and the District Court and toss out the entire ACA on the specious ground that Congress wouldn't want the ACA to survive without the individual mandate. The premise -- that there is no longer an individual mandate -- flies in the face of the fact that the ACA still contains the individual mandate. The penalty for not purchasing health-insurance coverage was reduced to $0 in the 2017 tax reform law, which renders the mandate a somewhat toothless requirement, But even before 2017, the IRS's collection tools under the ACA were quite limited, which rendered the individual mandate one of the most under-enforced requirements in the United States Code.
Even if the Court agrees that the individual mandate is no more, however, the idea that the Court would go along with tossing out the entire ACA is mind-boggling. That would mean:
- no more prohibition against pre-existing condition exclusions
- no more prohibition against arbitrary and discriminatory rescissions
- no more family coverage for children up to age 26
- the reintroduction of annual and lifetime caps on coverage
- no more Medicaid expansion funds (raising a serious question about the status of funds for the 39 states that have expanded eligibility based on a promise of a generous (read: massive) federal subsidy)
- the elimination of federal insurance exchanges and possibly state exchanges, too
- the elimination of premium tax credits for low-income households
- the elimination of subsidies for out-of-pocket expenditures
- the elimination of what amounts to a cap on the amount insurers can spend on items other than health-care claims (accompanied by a premium rebate when non-health-care expenditures exceed the permitted amount)
- and on and on and on.
Tuesday, May 25, 2021
COVID-19 at the Intersection of Criminal Justice Reform and Public Health
As jails and prisons remain leading sites of COVID-19 outbreaks, mass incarceration poses ongoing health risks for communities. We investigate whether short-term jailing of individuals prior to release may drive COVID-19 spread. We find that cycling individuals through Cook County Jail in March 2020 alone can account for 13% of all COVID-19 cases and 21% of racial COVID-19 disparities in Chicago as of early August. We conclude that detention for alleged offenses that can be safely managed without incarceration is likely harming public safety and driving racial health disparities. These findings reinforce consensus among public health experts that large-scale decarceration should be implemented to protect incarcerated people, mitigate disease spread and racial disparities, and improve biosecurity and pandemic preparedness.
The full article is well worth a close read.
Monday, May 24, 2021
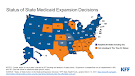
Texas Blows it Again on Medicaid Expansion
Health Affairs has posted a nice summary of the Biden Administration's attempt to entice the hold-out states to expand Medicaid pursuant to the ACA (though it unfortunately has absolutely no relevance to Texas -- read on):
In the newest addition to our “Eye On Health Reform” series, Katie Keith covers the American Rescue Plan Act, which was signed into law by President Joe Biden in March.
Keith explains that the legislation temporarily expands the Affordable Care Act’s premium tax credits and increases federal financial incentives for holdout states to expand their Medicaid programs. Keith also explores enrollment trends in states that use HealthCare.gov, current ACA litigation, and ACA guidance from the Biden administration.
I wrote about an earlier plan to pay hold-outs on Feb. 16, back when the prospects for expansion in Texas seemed, if not bright, at least alive. By my count there were five House bills, two Senate bills, four House Joint Resolutions, and three Senate Joint Resolutions that would have authorized (or required) Texas to take advantage of the federal dollars that would become available if Texas were to expand Medicaid eligibility to 138% of the federal poverty limit. Would it be cynical of me -- or simply realistic -- to report that every single one of these proposals died in committee? Every one! What is there to say other than it really sucks to be poor and live in Texas, where the legislature seems determined to keep a minimum level of health care out of reach for five million of its citizens.
For the record, here are the links to the bills and JRs, along with the names of co-sponsors:
HJR 9, 23, 24, 86
SJR 11, 14, 15
HB 143, 398, 513, 1730, 4406
SB 38, 119
Tuesday, May 11, 2021
"What Has President Biden Done in Health Care Coverage in His First 100 Days?"
Tuesday, March 23, 2021
AstraZeneca in Major Dispute with U.S. Regulators
Late Monday, the Data and Safety Monitoring Board (DSMB) notified NIAID, BARDA, and AstraZeneca that it was concerned by information released by AstraZeneca on initial data from its COVID-19 vaccine clinical trial. The DSMB expressed concern that AstraZeneca may have included outdated information from that trial, which may have provided an incomplete view of the efficacy data. We urge the company to work with the DSMB to review the efficacy data and ensure the most accurate, up-to-date efficacy data be made public as quickly as possible.
It is almost (but not quite) inconceivable that AstraZeneca made an innocent error. The DSMB is accusing the firm of essentially "cherry-picking" the data “most favorable for the study as opposed to the most recent and most complete.” (NY Times, 3/23) The DSMB's letter to the NIH and AstraZeneca stated that the efficacy rate of the firm's COVID-19 vaccine might be between 69% and 74%, rather than the 79% rate touted by AstraZeneca itself. Did AstraZeneca really think they could slip one past the regulators? And at what cost to its reputation? Not to mention at what cost to the worldwide public-health crisis, where mistrust of science and vaccine-skepticism don't need any more encouragement and support.
From the Times article: “'Decisions like this are what erode public trust in the scientific process,' the board wrote."
Monday, March 22, 2021
Medicaid Expansion in Texas: The Time is Now
The Legislature is back in session. A bill has been introduced to authorize Texas to accept the federal government's offer to pay for 90% of the cost of expanding Medicaid eligibility to include all Texans under the age of 65 (when Medicare kicks in) and whose income does not exceed 138% of the federal poverty level: HB 1730, introduced by Republican Representative Lyle Larson. Sen. Johnson's own companion bills are SB 118 and SB 119.
The case for expansion is made in a most compelling and entertaining video (10.5 minutes) by Senator Nathan Johnson (D-Dist. 16 (which covers a big chunk of Dallas)). Please watch it. Share it with your family. Send it to your friends. Get involved. We have already waited too long, left billions of federal dollars on the table, and worst of all, we've ignored the health care needs of 1 million Texans who would benefit from expansion. Let's make this happen this year.
And thanks to DFW Hospital Council CEO Stephen Love for passing the video on to me.
Monday, March 08, 2021
CDC's Guidance for "Fully Vaccinated People"
The guidance was issued earlier today, and you can read the whole document here. Meanwhile, here are the highlights:
Key Points
This is the first set of public health recommendations for fully vaccinated people. This guidance will be updated and expanded based on the level of community spread of SARS-CoV-2, the proportion of the population that is fully vaccinated, and the rapidly evolving science on COVID-19 vaccines.
For the purposes of this guidance, people are considered fully vaccinated for COVID-19 ≥2 weeks after they have received the second dose in a 2-dose series (Pfizer-BioNTech or Moderna), or ≥2 weeks after they have received a single-dose vaccine (Johnson and Johnson [J&J]/Janssen ).†
The following recommendations apply to non-healthcare settings.
Fully vaccinated people can:
Visit with other fully vaccinated people indoors without wearing masks or physical distancing
Visit with unvaccinated people from a single household who are at low risk for severe COVID-19 disease indoors without wearing masks or physical distancing
Refrain from quarantine and testing following a known exposure if asymptomatic
For now, fully vaccinated people should continue to:
Take precautions in public like wearing a well-fitted mask and physical distancing
Wear masks, practice physical distancing, and adhere to other prevention measures when visiting with unvaccinated people who are at increased risk for severe COVID-19 disease or who have an unvaccinated household member who is at increased risk for severe COVID-19 disease
Wear masks, maintain physical distance, and practice other prevention measures when visiting with unvaccinated people from multiple households
Avoid medium- and large-sized in-person gatherings
Get tested if experiencing COVID-19 symptoms
Follow guidance issued by individual employers
Follow CDC and health department travel requirements and recommendations
Thursday, March 04, 2021
Free Webinar: Pres. Biden's First 100 Days of Health Policy
Boston University's Center for Health Law, Ethics & Human Rights faculty discuss the first 100 days of President Biden’s term:
- Executive Orders,
- proposed bills, and
- other steps to tackle COVID, climate, and economic crises affecting health.
1:00 - 2:30 p.m. EST
SPEAKERS
George Annas
Nicole Huberfeld
Wendy Mariner
Michael Ulrich
JOIN ZOOM MEETING
https://bostonu.zoom.us/j/93372687004?pwd=NXpoNm5wZW1YOEljeENyeWY2V3dVUT09
Meeting ID: 933 7268 7004
Passcode: 331167
Tuesday, March 02, 2021
"Governor Abbott Lifts Mask Mandate, Opens Texas 100 Percent" [source: Governor's website]
Yes, it's true. Governor Abbott (along with the Governor of Mississippi) has earned the title "Worst Public Health Decision Maker Still Holding Office in the U.S." with this announcement. The full text of Executive Order GA-34 is here.
Gov. Abbott offered remarks on his remarkable EO in Lubbock. Here is an annotated paragraph:
"With the medical advancements of vaccines and antibody therapeutic drugs, Texas now has the tools to protect Texans from the virus,” said Governor Abbott.
You bet we have the tools. We simply have to use them.
"Make no mistake, COVID-19 has not disappeared, but it is clear from the recoveries, vaccinations, reduced hospitalizations, and safe practices that Texans are using that state mandates are no longer needed."
Wow, that's a whopper. To borrow a line from Justice Ginsburg's dissent in Shelby County, in which the majority held that the Voting Rights Act's preclearance mechanism was no longer needed: "Throwing out preclearance when it has worked and is continuing to work to stop discriminatory changes is like throwing away your umbrella in a rainstorm because you are not getting wet." [Opinion, p. 33]
"Today's announcement does not abandon safe practices that Texans have mastered over the past year."
Another whopper. Texans haven't mastered safe practices and now we've been given a green light to abandon them altogether.
"Effective next Wednesday [Mar. 10], all businesses of any type may open to 100% capacity." "This order ends the statewide mask mandate in Texas."
Abbott helpfully notes that anyone who wants to can wear a mask and businesses can self-limit their own capacity. That's the kind of right-thinking Texas policy that gave us ERCOT and the disaster of two weeks ago. We are going our own way and celebrating Texas independence. Wonderful spirit, but lots of people died. And lots of people are going to die of COVID-19 unnecessarily because of today's order.
Stephen Love, the President/CEO of the Dallas-Fort Worth Hospital Council had this to say:
"While we respect Governor Greg Abbott and realize he has faced enormous challenges with the COVID-19 pandemic and recent weather issues, we strongly disagree with removing the mandatory mask requirements. This decision will cause the community spread to increase, forcing our exhausted healthcare heroes to diagnose, treat and save the lives of newly infected patients. If the community spread increases, the risk of mutations will also increase, creating a new set of potentially dangerous challenges. If you truly want to honor our healthcare heroes, then continue to wear a mask! We ask Governor Abbott to please reconsider his decision."
Back to the governor:
"Instead, it is a reminder that each person has a role to play in their own personal safety and the safety of others."
Agreed. What the Executive Order ignores is that the state has a role to play, as well. And the governor has just abandoned that responsibility.
"With this executive order, we are ensuring that all businesses and families in Texas have the freedom to determine their own destiny."
And the destiny of all others -- family, workers, strangers -- with whom they come into contact. Gulp.
Sunday, February 21, 2021
COVID-19 Vaccination and Ethics: Stanford/AJOB Webinar
The American Journal of Bioethics and Stanford's Center for Biomedical Ethics (David Magnus & Bela Fishbeyn) on Feb. 16 put on an excellent panel discussion of the ethics of COVID-19 vaccination policies. It was a far-ranging discussion with knowledgeable participants and well worth watching.
Saturday, February 20, 2021
Medicaid in Times of Crisis: A GAO Report (2 pp.)
It's short but sweet. The Government Accountability Office has issued GAO-21-343SP (02-17-2021), a nifty description and analysis of the role of the federal-state Medicaid program in times of crisis (e.g., epidemics and pandemics, economic recessions, natural disasters, and personal health crises). Specific examples over the past 15 years include Hurricane Katrina, the Great Recession, the opioid epidemic, and of course COVID-19.
This is further proof, as if any were needed, that Texas's policy of not expanding Medicaid eligibility at largely federal expense isn't only hurting the indigent (and largely minority) individuals -- including millions of kids -- that legislators seem keen to punish for being, you know, indigent, nonwhite, and young. The policy is also depriving public-health officials of an important tool in times of great public need.
Thursday, February 18, 2021
COVID Vaccine and Health Equity: We have a long way to go
From Kaiser Health News (2/18/2021):
KFF has an updated analysis of state-reported data as of February 16, 2021 on COVID-19 vaccinations, cases, and deaths by race/ethnicity.
New to the analysis are comparisons of vaccination rates in each racial/ethnic group based on state-reported data of total people who have received at least one dose of the vaccine. Among just over half of states reporting data, the vaccination rate among White people is over three times higher than the rate for Hispanic people (10% vs 3%) and twice as high as the rate for Black people (10% vs. 5%). The vaccination rate for Asian people is closer to the rate for White people in most reporting states, although they are less likely to have been vaccinated in most reporting states.
Wednesday, February 17, 2021
Planned Parenthood, Medicaid Expansion, and Women's Health
Another example of weaponization was pointed out in an op-ed in the New York Times (02-17-2021) by Dr. Samuel Dickman, an internist and the medical director for primary care at Planned Parenthood South Texas:
For the past several years, Texas politicians have worked to cut off Medicaid recipients’ access to the wide range of services offered by Planned Parenthood. Now, barring an extension of a state district court’s temporary block on their efforts, they may have gotten their way.
Gov. Greg Abbott, a Republican, and like-minded state officials targeted Planned Parenthood because it offers abortion services. But abortion services account for just a fraction of the care we provide, which means the consequences of a new policy would be far more sweeping.
If it goes into effect, this policy would block patients’ access to blood pressure checks, cancer screenings, birth control, S.T.D. treatment and other medical care routinely provided at Planned Parenthood health centers in Texas, where I serve as a medical director for primary care. Nationally these other essential services, not abortion care, account for 96 percent of Planned Parenthood’s patient visits; in Texas, for example, some 24,000 Medicaid patients received non-abortion care over the past four years.
The aforementioned cruel and punitive nature of the proposed change should be obvious:
States’ denials of health care coverage, including Texas’ refusal to expand Medicaid, contributed to 461,000 excess deaths in 2018 that would have been averted if the United States had kept up with other wealthy countries, a tragedy documented in a report by my colleagues and me published this month in The Lancet.
It is also just bad policy. Not just bad health policy, which it obviously is, but bad fiscal policy as well. Untreated STDs will increase the cost of health care because of expensive later treatments. Forgone cancer screenings, untreated hypertension and a host of other chronic conditions only get more expensive the longer preventive care is postponed denied once Planned Parenthood is knocked out of the Medicaid program altogether. Gov. Abbott and his pals have to be stopped. If they aren't, any Medicaid expansion that Texas may stumble into (see yesterday's post) will leave these 24,000 women and many others in years to come out in the cold.
Tuesday, February 16, 2021
Medicaid Expansion: Biden's COVID Relief Proposal Includes a Cash Sweetener for Texas and 11 Other Holdouts
As reported by The Washington Post (02/16/21), the 5,593-page COVID relief bill supported by the Biden Administration contains a provision to increase Medicaid reimbursements by 5 percent for holdout states that finally do the right thing and expand Medicaid eligibility to 133 percent of the federal poverty line. Some excerpts from the Post's article:
Texas has more uninsured residents than any other state — partly because the massive state has spurned expansion. That means no Medicaid for most adults earning up to 133 percent of the federal poverty level (around $17,000 for a single person or $35,000 for a family of four). . . .
A coronavirus relief bill working its way through Congress and backed by President Biden includes a hefty incentive for states to expand Medicaid. If a state did so, the federal government would increase its Medicaid contribution to the state by 5 percent. The increased match rate would apply to everyone outside the expansion group and would last two years.
For Texas, that would mean nearly $6 billion extra dollars in Medicaid funds over two years. . . .
It appears that a handful of Republican legislators -- and even Governor Abbott -- may be warming to the idea of accepting billions of federal dollars in order to provide decent health care to over 5 million uninsured Texans (that's 17.7% of the population, more than double the national rate of uninsured (8.5%).
This shouldn't even be debatable. But maybe, just maybe, the times (and the state) are a-changin'. San Antonio's Republican Representative Lyle Larson has introduced HB 1730, a bill "[r]elating to the expansion of eligibility for Medicaid to all persons for whom federal matching money is available." Fingers crossed.