JAMA has published a free online article,
"Maternal Mortality Crisis and Extension of Medicaid Postpartum Coverage", but before reading this valuable article, I strongly recommend
the accompanying video that explores the reasons for this country's dismal record and the resulting tsunami of individual and family suffering and misery. For an investment of a mere 30 minutes, this video offers a lot of lessons, busts dangerous myths that surround maternal mortality. It's a deep and subtle dive into causes and possible solutions. For starters, JAMA's Editor-in-Chief, Kirsten Bibbins-Domingo, PhD, MD, MAS, introduces three take-aways with this comment: "A recent release from the
National Center for Health Statistics in March of 2023, covered by JAMA Medical News, makes the case for the importance of this issue with the numbers in the US from 2021. There are three things that are striking in the numbers on maternal mortality in the US."
- The first is that they're high. The US rate for 2021 was 32.9 maternal deaths per a hundred thousand live births. This is a number more than 10 times the estimated rates for other high income countries. Countries like Australia, Austria, Israel, Japan, and Spain, all hover between two to three deaths per a hundred thousand live births.
- The second important point is that the numbers are strikingly high in particular populations in the US, most notably Black women whose mortality rates are more than two and a half times that of white women. Hispanic women's mortality rates are at an all time high and surpassing those of white women. For other populations without appropriate data collection, we can't quantify the disparities accurately, and this is needed if we are to design interventions and allocate resources across all communities and populations. For example, data regarding American Indian women are rarely highlighted even though they have a high prevalence of poor outcomes. And in Asian populations, data disaggregation is needed to understand and interpret the true trends.
- The third important point, the one that really got to me in this new report, is that the trends are getting worse. More than 1200 people died of maternal causes in the US in 2021, a 40% increase from the previous year. And in every group examined in this new report across all races and ethnicities, across all ages of pregnant people, the trends are getting worse over time.
The Q&A that follows brings together three women who are practicing physicians, researchers, or both. It's an incredibly insightful colloquy.
This is prelude to the article cited above by Eli Y. Adashi, MD, MS; Daniel P. O’Mahony, MSLS; I. Glenn Cohen, JD. The point I want to emphasize is the connection between the mortality crisis and the law, specifically Medicaid.
The video panelists all seem to agree that the post-partum period is the most lethal yet the one where our healthcare "system" fails women:
One in 3 pregnancy-associated deaths occur within 1 year of childbirth. Thus the extension of Medicaid postpartum coverage from 60 days (the duration required by federal law) to 12 months has emerged as a key strategy to address the US maternal mortality crisis.2 This Viewpoint assesses the maternal mortality crisis in the US, calls for an extension of Medicaid postpartum coverage, and discusses the residual challenges across the US related to maternal health.
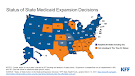
States are currently free to extend post-partum coverage of their Medicaid programs, but not many have done so. Of particular interest to Texans and others who live in states whose legislatures and governors have not expanded Medicaid eligibility pursuant to Obamacare's generous federal match, the situation is even worse:
Although some individuals may qualify for extended postpartum Medicaid coverage because of their economic circumstances (ie, those with incomes ≤138% of the federal poverty level), many others are likely to no longer be eligible for Medicaid coverage, especially in the states that have not expanded Medicaid coverage.3 Postpartum individuals who reside in nonexpansion states can only qualify for Medicaid as parents.3 However, Medicaid income eligibility levels for parents are much lower than those for pregnant people.3 It follows that many individuals living in nonexpansion states become uninsured after their pregnancy-related coverage ends at 60 days’ postpartum.
How on earth can this continue?